Disease ⸺ Hydrocephalus with Skeletal Anomalies
Overview of Hydrocephalus and Skeletal Anomalies
Hydrocephalus is a disorder characterized by an abnormal accumulation of cerebrospinal fluid within the brain’s ventricles‚ leading to increased intracranial pressure․ Skeletal anomalies‚ including malformations in the skull or spine‚ are congenital defects that can be associated with hydrocephalus․ These anomalies can impact the development of the central nervous system and result in neurological impairments․
Congenital hydrocephalus with skeletal abnormalities is a complex condition that requires specialized medical care․ The growth and function of the skull‚ spine‚ and brain are intricately linked‚ making the co-occurrence of these abnormalities significant․ Understanding the interplay between hydrocephalus and skeletal anomalies is crucial for effective diagnosis and management․
Individuals with hydrocephalus and skeletal anomalies may experience a range of comorbidities and symptoms related to both conditions․ Early diagnosis is essential to prevent further complications and address developmental challenges․ Treatment approaches often involve a multidisciplinary team of healthcare professionals to provide comprehensive care tailored to the specific needs of the patient․
By exploring the impact of hydrocephalus with skeletal anomalies on growth‚ neurological function‚ and overall well-being‚ healthcare providers can develop personalized treatment plans to improve outcomes and enhance the quality of life for affected individuals․ Continued research and advancements in medical technology play a vital role in advancing the understanding and management of this complex disease․
Causes of Hydrocephalus with Skeletal Anomalies
The causes of hydrocephalus with skeletal anomalies are multifaceted and can involve a combination of genetic‚ environmental‚ and developmental factors․ Congenital hydrocephalus‚ often present at birth‚ may result from abnormalities in the development of the brain and spinal cord‚ leading to impaired cerebrospinal fluid circulation․
Genetic conditions such as Dandy-Walker syndrome‚ Chiari malformation‚ and spina bifida are known to be associated with hydrocephalus and skeletal anomalies․ These conditions can affect the formation of the skull‚ spine‚ and neural tube‚ contributing to the development of structural defects that impact normal growth and function․
Acquired hydrocephalus‚ which can occur due to conditions such as infections‚ tumors‚ or hemorrhages‚ may also be linked to skeletal abnormalities․ Disruptions in the flow or absorption of cerebrospinal fluid can lead to an increased accumulation within the ventricular system‚ exacerbating the pressure on the brain and potentially affecting skeletal development․
Additionally‚ certain developmental disorders or injuries during fetal development can disrupt the intricate process of skeletal formation and brain growth‚ resulting in a complex interplay between hydrocephalus and skeletal anomalies․ Understanding the underlying causes of these conditions is essential for accurate diagnosis and tailored treatment strategies․
By investigating the specific etiological factors contributing to hydrocephalus with skeletal anomalies‚ healthcare providers can better address the unique needs of each patient and provide comprehensive care aimed at optimizing outcomes and minimizing complications associated with these complex conditions․
Impact on Growth and Neurological Impairment
Hydrocephalus with skeletal anomalies can have a profound impact on both growth and neurological function․ The abnormal accumulation of cerebrospinal fluid within the brain’s ventricles can exert pressure on surrounding structures‚ affecting the growth and development of the skull and spine․ This may lead to structural malformations that influence overall growth patterns and skeletal alignment․
Furthermore‚ the presence of skeletal anomalies in conjunction with hydrocephalus can contribute to neurological impairment․ As the central nervous system interacts closely with the skeletal framework‚ disruptions in skeletal development can have cascading effects on neurological function․ The compression or distortion of neural pathways due to abnormal skeletal structures may result in motor deficits‚ sensory issues‚ and cognitive challenges․
In children with hydrocephalus and skeletal anomalies‚ the interplay between these conditions can impact milestones of growth and development․ Skeletal deformities may necessitate specialized care to promote proper alignment and mobility‚ while neurological impairments may require targeted interventions to address cognitive delays or motor limitations․
Recognizing the complex relationship between growth‚ skeletal anomalies‚ and neurological function is crucial for healthcare providers when evaluating and managing individuals with hydrocephalus and associated skeletal abnormalities․ By monitoring growth parameters‚ assessing neurological milestones‚ and addressing both the skeletal and neurological components of the condition‚ healthcare teams can work collaboratively to optimize outcomes and enhance the quality of life for affected individuals․
Diagnosis and Symptoms
Diagnosing hydrocephalus with skeletal anomalies involves a comprehensive evaluation that includes a detailed medical history‚ physical examination‚ and diagnostic imaging studies․ Symptoms of hydrocephalus can vary and may include signs of increased intracranial pressure such as headaches‚ nausea‚ vomiting‚ and visual disturbances․
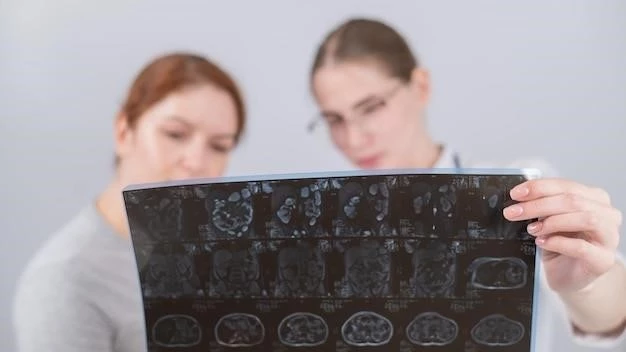
Additional symptoms related to skeletal anomalies may manifest as abnormal skull shape‚ spinal deformities‚ or limb abnormalities․ Imaging modalities such as ultrasound‚ CT scans‚ or MRI scans are commonly used to assess the structure of the brain‚ skull‚ and spine to detect any abnormalities or malformations present․
In infants and young children‚ early signs of hydrocephalus and skeletal anomalies may be identified through developmental delays‚ changes in head circumference‚ or motor deficits․ Collaboration between pediatric neurologists‚ orthopedic specialists‚ and radiologists is essential to accurately diagnose and characterize the extent of the condition․
Other diagnostic tests‚ such as genetic testing for associated syndromes or metabolic disorders‚ may be recommended to further elucidate the underlying etiology of the condition․ By carefully correlating clinical symptoms with imaging findings and specialized tests‚ healthcare providers can formulate a precise diagnosis and develop a tailored treatment plan for each individual․
Timely and accurate diagnosis of hydrocephalus with skeletal anomalies is critical for initiating appropriate interventions to address symptoms‚ prevent complications‚ and optimize long-term outcomes․ Effective communication among healthcare professionals‚ patients‚ and families is key to ensuring comprehensive care and support throughout the diagnostic process and treatment journey․
Treatment Approaches
The treatment of hydrocephalus with skeletal anomalies often requires a multidisciplinary approach involving neurosurgeons‚ orthopedic surgeons‚ pediatric specialists‚ and rehabilitation therapists․ The primary goal of treatment is to alleviate symptoms‚ improve quality of life‚ and address any associated complications․
Surgical interventions‚ such as the insertion of a ventriculoperitoneal shunt to drain excess cerebrospinal fluid or the correction of skeletal deformities through orthopedic procedures‚ may be necessary depending on the specific manifestations of the conditions․ These procedures aim to relieve pressure on the brain‚ restore normal cerebrospinal fluid circulation‚ and optimize skeletal alignment․
Regular monitoring and follow-up care are essential components of the treatment plan to ensure the effectiveness of interventions and to address any emerging issues promptly․ Physical therapy‚ occupational therapy‚ and other rehabilitative measures may be prescribed to help individuals with hydrocephalus and skeletal anomalies improve mobility‚ strength‚ and overall function․
Pharmacological management‚ including the use of medications to control symptoms such as pain or muscle spasticity‚ may complement surgical and rehabilitative interventions․ Close collaboration between healthcare providers and families is crucial to tailor treatment approaches to the unique needs and circumstances of each individual․
Educating patients and caregivers about the conditions‚ treatment options‚ and potential outcomes is vital for informed decision-making and active participation in the care process․ By combining medical expertise with holistic support‚ healthcare teams can work collaboratively to address the complex challenges associated with hydrocephalus and skeletal anomalies‚ striving to enhance the well-being and quality of life of those affected․
Prognosis and Rehabilitation
The prognosis for individuals with hydrocephalus and skeletal anomalies varies depending on the severity of the conditions‚ response to treatment‚ and presence of comorbidities․ Early diagnosis and intervention play a crucial role in determining outcomes and minimizing long-term complications․
While some individuals may experience significant improvements in symptoms and functional abilities with appropriate treatment‚ others may face ongoing challenges related to neurological impairment‚ skeletal deformities‚ or developmental delays․ Rehabilitation strategies‚ including physical and occupational therapy‚ can help optimize independence‚ mobility‚ and quality of life․
Long-term management of hydrocephalus and skeletal anomalies requires regular monitoring‚ follow-up care‚ and adjustments to the treatment plan as needed․ Healthcare providers collaborate closely with patients and families to address evolving needs‚ promote holistic well-being‚ and provide ongoing support throughout the rehabilitation process․
Prognostic factors‚ such as the underlying etiology of the conditions‚ the presence of associated syndromes‚ and the individual’s overall health status‚ significantly influence the long-term outlook․ By emphasizing comprehensive rehabilitation and supportive care‚ healthcare teams strive to enhance the prognosis and quality of life for individuals living with hydrocephalus and skeletal anomalies․
In conclusion‚ the co-occurrence of hydrocephalus with skeletal anomalies presents a complex clinical scenario that necessitates a multidisciplinary approach for diagnosis‚ treatment‚ and ongoing management․ Understanding the intricate relationship between these conditions is essential for providing personalized care and optimizing outcomes for affected individuals․
Early recognition of symptoms‚ prompt diagnostic evaluation‚ and tailored treatment interventions are paramount in addressing the unique challenges posed by hydrocephalus and skeletal anomalies․ Collaboration among neurosurgeons‚ orthopedic specialists‚ rehabilitation therapists‚ and other healthcare professionals is crucial for delivering comprehensive care that addresses both the neurological and musculoskeletal aspects of the conditions․
Rehabilitation efforts aimed at enhancing mobility‚ function‚ and quality of life play a vital role in the long-term care of individuals with hydrocephalus and skeletal anomalies․ By combining medical expertise with rehabilitative strategies and ongoing support‚ healthcare teams can empower patients to thrive and overcome the challenges associated with these complex conditions․
Continued research‚ advancements in treatment modalities‚ and a patient-centered approach are key to improving the prognosis and quality of life for individuals living with hydrocephalus and skeletal anomalies․ By prioritizing holistic care‚ education‚ and empowerment‚ healthcare providers can make a meaningful difference in the lives of those affected by these challenging conditions․
