The negative rheumatoid factor polyarthritis is characterized by the absence of specific antibodies in the patient’s blood, distinct from seropositive rheumatoid arthritis.
Definition and Characteristics
Negative rheumatoid factor polyarthritis is primarily identified by the absence of rheumatoid factor antibodies in the blood, setting it apart from seropositive forms of arthritis. This subtype often presents challenges in diagnosis and treatment due to the lack of specific antibodies typically associated with rheumatoid arthritis.
Laboratory Tests for Diagnosis
Useful laboratory tests for patients with polyarthritis may include a complete blood count, erythrocyte sedimentation rate, rheumatoid factor test, and more to aid in diagnosis and treatment.
Useful Tests for Patients with Polyarthritis
When diagnosing polyarthritis, healthcare providers may utilize various laboratory tests to aid in the diagnostic process. Common tests include a complete blood count, erythrocyte sedimentation rate, C-reactive protein test, rheumatoid factor test, and anti-cyclic citrullinated peptide antibody test to help identify and differentiate between different types of arthritis.
Seronegative Rheumatoid Arthritis
Seronegative rheumatoid arthritis is characterized by the absence of certain antibodies in the patient’s blood, distinguishing it from seropositive forms of the condition.
Understanding Seronegative Rheumatoid Arthritis
Seronegative rheumatoid arthritis is a distinct subtype characterized by the absence of specific antibodies like rheumatoid factor and anti-cyclic citrullinated protein. This subset poses diagnostic challenges due to the lack of these antibodies often associated with rheumatoid arthritis.
Rheumatoid Factor in Autoimmune Diseases
Rheumatoid factor is a protein that can attack healthy tissue, often present in autoimmune diseases like rheumatoid arthritis and Sjogren syndrome.
Role of Rheumatoid Factor in Autoimmune Conditions
The presence of rheumatoid factor in the blood is a hallmark of certain autoimmune diseases, particularly rheumatoid arthritis. This protein can indicate the immune system’s attack on healthy tissue, playing a crucial role in the diagnosis and management of autoimmune conditions.
Polyarthritis refers to inflammation in at least five joints simultaneously and can stem from various conditions, including autoimmune diseases like rheumatoid arthritis and infections.

Polyarthritis and its Causes
Polyarthritis, characterized by inflammation in at least five joints simultaneously, can arise from various conditions, including autoimmune diseases like rheumatoid arthritis, infections, and systemic vasculitis among others.
RF-positive polyarthritis is a subtype of juvenile idiopathic arthritis characterized by the presence of rheumatoid factor in the blood, usually within the first 6 months of onset.
Subtypes of JIA ⎼ RF-Positive Polyarthritis
RF-positive polyarthritis, a subtype of juvenile idiopathic arthritis, is defined by the presence of rheumatoid factor in the blood, indicating autoimmune activity typically seen in the early stages of the disease.
RF-Negative Polyarthritis in JIA
RF-negative polyarthritis in Juvenile Idiopathic Arthritis (JIA) is characterized by arthritis in at least five joints within the first six months, but without the presence of rheumatoid factor in the blood.
Description of RF-Negative Polyarthritis
RF-negative polyarthritis in Juvenile Idiopathic Arthritis (JIA) is characterized by arthritis in at least five joints within the first six months, but without the presence of rheumatoid factor in the blood. This subset presents challenges in diagnosis and management due to the absence of this specific autoimmune marker.
Diagnostic Testing and Seronegativity
Diagnostic testing for seronegative conditions in arthritis involves assessing factors like rheumatoid factor and anti-cyclic citrullinated protein to understand disease characteristics and guide treatment decisions.
Importance of Diagnostic Testing for Seronegative Conditions
Diagnostic testing for seronegative conditions such as rheumatoid factor-negative polyarthritis plays a crucial role in identifying and differentiating autoimmune diseases like rheumatoid arthritis. These tests help healthcare professionals understand the disease characteristics, guide treatment decisions, and improve overall patient outcomes.
Juvenile Idiopathic Arthritis (JIA)
Juvenile Idiopathic Arthritis (JIA) encompasses a group of chronic disorders characterized by arthritis persisting for at least 6 weeks with onset before the age of 16. Within this classification٫ JIA’s polyarticular form further divides based on the presence of rheumatoid factor.
Overview of JIA and Polyarticular Forms
Juvenile Idiopathic Arthritis (JIA) encompasses chronic disorders with arthritis persisting for at least 6 weeks, usually before age 16. Within this cluster, polyarticular JIA forms based on the presence of rheumatoid factor, dividing the condition into distinct subtypes for diagnosis and treatment.
Management and Treatment Approaches
Managing negative rheumatoid factor polyarthritis involves a multifaceted approach utilizing medications, physical therapy, lifestyle modifications, and regular monitoring to alleviate symptoms and improve quality of life for affected individuals.
Juvenile Idiopathic Arthritis (JIA)
Juvenile Idiopathic Arthritis (JIA) comprises a group of chronic disorders characterized by arthritis persisting for at least 6 weeks with onset before age 16. This classification further divides into polyarticular forms based on certain antibodies in the blood.
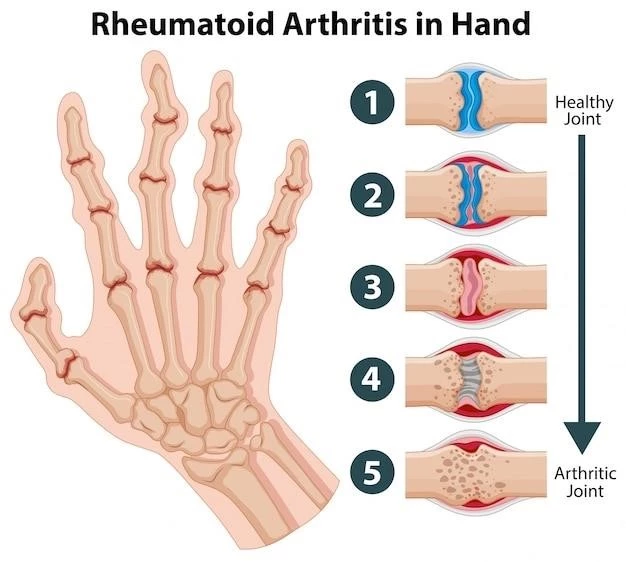
Impact on Physical Function
Negative rheumatoid factor polyarthritis can severely impact physical function, leading to joint damage and reduced mobility, affecting daily activities and overall quality of life.
Consequences of Untreated Polyarthritis
Untreated polyarthritis can lead to joint damage, disability, reduced physical function, and diminished quality of life. Early diagnosis and appropriate management are crucial to prevent long-term complications.
Risk Factors and Prognosis
Factors such as age, family history of autoimmune diseases, smoking, and environmental triggers may contribute to the risk of negative rheumatoid factor polyarthritis. Prognosis varies depending on early diagnosis and the effectiveness of treatment.
Serological Status as a Prognostic Indicator
Serological status, characterized by the presence or absence of rheumatoid factor (RF) and anti-cyclic citrullinated peptide antibody (ACPA), serves as a significant diagnostic and prognostic factor in autoimmune diseases like rheumatoid arthritis. The absence of these antibodies, known as seronegative status, presents challenges in diagnosis and treatment planning, impacting the overall disease course.
Research and Future Directions
Recent research is focusing on understanding the pathophysiology of negative rheumatoid factor polyarthritis, exploring novel treatment approaches, and investigating potential biomarkers for improved diagnosis and prognosis. Future directions include personalized medicine strategies and advancements in targeted therapies for better management of this condition.
Advancements in Understanding RF-Negative Polyarthritis
Ongoing research efforts are aimed at enhancing our comprehension of RF-negative polyarthritis, including exploring novel treatment modalities, investigating potential biomarkers for refined diagnosis and prognosis prediction, and advancing personalized medicine strategies tailored to the specific needs of individuals with this condition. These advancements hold promise for improving the overall management and outcomes of patients with negative rheumatoid factor polyarthritis.
