Introduction to Portal Vein Thrombosis
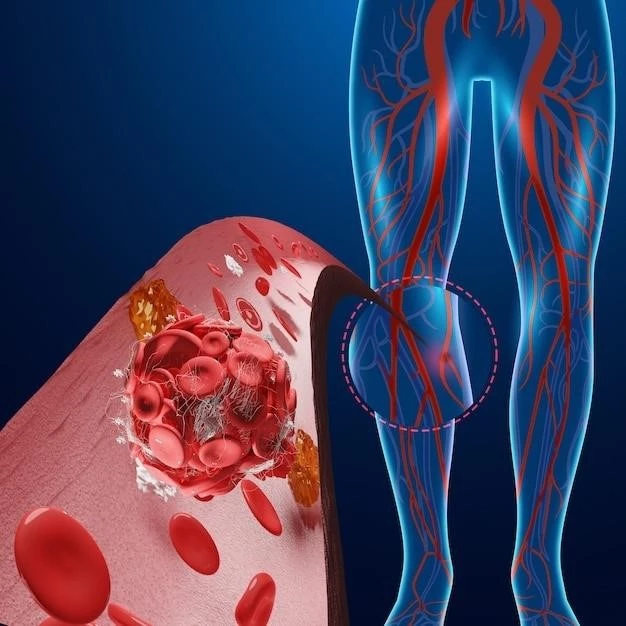
Portal vein thrombosis, also known as PVT, refers to the blockage or narrowing of the portal vein by a blood clot. This condition can lead to increased pressure in the portal vein system and reduced blood supply to the liver. It is commonly associated with liver cirrhosis but can also occur in the absence of cirrhosis with various complications. Prompt diagnosis and management of PVT are crucial to prevent serious consequences.
Definition and Overview
Portal vein thrombosis, or PVT, is often characterized by the obstruction or constriction of the portal vein due to a blood clot. This condition can lead to elevated pressure in the portal vein system and reduced blood flow to the liver. Typically linked with liver cirrhosis, PVT can also manifest without underlying liver disease, posing various complications. Timely identification and management of PVT are critical to prevent adverse outcomes.
Causes and Risk Factors
The causes of portal vein thrombosis can vary, with the most common cause being related to slow or scarred blood flow through the liver. This condition is often associated with liver cirrhosis but can also occur due to other factors such as malignancies or metabolic and autoimmune diseases; Understanding the diverse range of causes and risk factors for portal vein thrombosis is crucial in its diagnosis and management.
Association with Liver Cirrhosis
Portal vein thrombosis often presents as a complication of liver cirrhosis, where a blood clot obstructs the portal vein, leading to increased pressure in the portal vein system. While commonly linked with cirrhosis, it can also occur independently of liver disease, though less frequently. Prompt diagnosis and management are vital to prevent adverse outcomes and complications associated with portal vein thrombosis in patients with liver cirrhosis.
Relationship to Solid Malignancy
Portal vein thrombosis can also be associated with solid malignancies, although it is less common compared to its association with liver cirrhosis. It is crucial to recognize the potential relationship between portal vein thrombosis and solid malignancies, as prompt diagnosis and management are essential to prevent severe complications and guide appropriate treatment strategies for patients with both conditions.

Symptoms and Diagnostic Methods
Portal vein thrombosis symptoms mainly include abdominal pain, nausea, vomiting, and gastrointestinal bleeding. Diagnosis involves Doppler ultrasonography to confirm the presence of blood clots in the portal vein. Prompt identification of symptoms and accurate diagnostic methods are crucial for timely intervention and management of portal vein thrombosis.
Clinical Presentation of Portal Vein Thrombosis
The clinical presentation of portal vein thrombosis commonly includes symptoms such as abdominal pain, nausea, vomiting, and gastrointestinal bleeding. In severe cases, patients may experience fever, sepsis, and lactic acidosis. Early recognition of these symptoms is vital for the timely diagnosis and management of portal vein thrombosis to prevent further complications.
Importance of Doppler Ultrasonography in Diagnosis
Doppler ultrasonography plays a crucial role in diagnosing portal vein thrombosis by confirming the presence of blood clots in the portal vein. This non-invasive imaging modality is essential for accurately detecting thrombosis and guiding appropriate treatment interventions. Early and precise diagnosis through Doppler ultrasonography is paramount to ensure timely management and minimize potential complications associated with portal vein thrombosis.
Complications and Prognosis
Complications of portal vein thrombosis include the impact on portal hypertension, which can lead to gastrointestinal bleeding and other serious consequences. Understanding chronic cavernous transformation, a common complication, is essential for prognosis evaluation and appropriate management strategies to prevent further complications and improve patient outcomes.
Impact on Portal Hypertension and Gastrointestinal Bleeding
Portal vein thrombosis can lead to portal hypertension, potentially resulting in severe complications such as variceal bleeding in the gastrointestinal tract. Understanding the relationship between portal hypertension and gastrointestinal bleeding is crucial in managing portal vein thrombosis to prevent life-threatening situations and improve patient outcomes.
Understanding Chronic Cavernous Transformation
Chronic cavernous transformation is a common complication of portal vein thrombosis characterized by the development of collateral vessels around the occluded portal vein. This transformation occurs over time as a response to blockage, helping to reroute blood flow. Understanding chronic cavernous transformation is crucial in assessing the severity of portal vein thrombosis and planning appropriate treatment strategies to manage the condition effectively.
When imaging portal vein thrombosis, emphasis is placed on the use of MRI to visualize the presence of blood clots within the portal vein. This imaging technique helps in identifying the extent and severity of thrombosis. Additionally, recognizing obliterative portal venopathy, a condition where the portal vein becomes obstructed, is crucial for accurate diagnosis and management of portal vein thrombosis.
Imaging Findings and Modalities
Portal vein thrombosis diagnosis often utilizes magnetic resonance imaging (MRI) to highlight the presence of blood clots within the portal vein. This imaging method is crucial for assessing the severity and extent of thrombosis. Furthermore, the identification of obliterative portal venopathy, a condition where the portal vein becomes obstructed, is fundamental for accurate diagnosis and effective management of portal vein thrombosis.
Recognition of Obliterative Portal Venopathy
Obliterative portal venopathy is characterized by the formation of collateral vessels around the occluded portal vein due to chronic portal vein thrombosis. This condition leads to rerouting of blood flow, contributing to the development of cavernous transformation. Recognizing obliteration portal venopathy is vital for understanding the chronic changes resulting from portal vein thrombosis and guiding appropriate treatment strategies.
Management and Treatment Approaches
Anticoagulation therapy plays a significant role in managing portal vein thrombosis. In cases where anticoagulation alone may not suffice, endovascular or surgical interventions become necessary. Prompt initiation of appropriate treatment strategies is essential to prevent potential complications and improve outcomes in patients with portal vein thrombosis.
Role of Anticoagulation in Portal Vein Thrombosis
Anticoagulation therapy plays a pivotal role in the management of portal vein thrombosis by preventing the formation and progression of blood clots within the portal vein. It is a primary treatment approach aimed at reducing the risk of clot-related complications and improving blood flow. Anticoagulants are essential in preventing further thrombus formation and promoting recanalization in patients with portal vein thrombosis.
Endovascular and Surgical Interventions
Endovascular and surgical interventions become necessary in some cases of portal vein thrombosis where anticoagulation therapy alone is insufficient. These approaches aim to manage complications, restore blood flow, and alleviate symptoms associated with portal vein thrombosis. It is essential to consider these interventions when determining the most effective treatment strategy for each individual patient.
