Understanding Portal Hypertension
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg.
Portal hypertension is an increase in pressure in the portal vein resulting from liver damage, leading to complications like varices and ascites. Common causes include cirrhosis, which obstructs blood flow through the liver.
Complications of Portal Hypertension
Portal hypertension leads to issues such as varices, ascites, hepatic encephalopathy, and liver failure.
Varices and Bleeding
Portal hypertension can result in the development of varices, which are enlarged veins in the esophagus and stomach. These varices are prone to rupture, leading to serious bleeding complications.
Ascites and Fluid Buildup
Portal hypertension can lead to the accumulation of fluid in the abdomen, a condition known as ascites. This buildup of fluid can result from the liver’s reduced ability to make proteins that help maintain fluid balance in the body.
Definition and Causes
Portal hypertension results from increased pressure in the portal vein due to conditions like cirrhosis obstructing blood flow through the liver.
Hepatic Venous Pressure Gradient
One key method of diagnosing portal hypertension is by measuring the hepatic venous pressure gradient, which is the pressure difference between the portal vein and the hepatic vein. This measurement helps determine the severity and assess the risk of complications associated with portal hypertension.
Imaging Techniques
Non-invasive imaging techniques such as ultrasound, CT scans, and MRI are used to assess the liver structure and identify complications of portal hypertension, like ascites and varices. These imaging modalities help in diagnosing and monitoring the progression of the condition while avoiding invasive procedures.
Management and Treatment Options
Portal hypertension is managed and treated using medications, endoscopic therapy, shunting procedures, and lifestyle changes.
Medications
Medications play a crucial role in managing portal hypertension, targeting factors like reducing blood pressure, preventing variceal bleeding, and improving liver function.
Endoscopic Therapy and Shunting Procedures
Endoscopic therapy and shunting procedures are commonly used to manage complications of portal hypertension like variceal bleeding by reducing portal pressure or redirecting blood flow to alleviate symptoms and prevent further complications.
Portal Hypertensive Gastropathy (PHG)
Portal hypertensive gastropathy (PHG) refers to changes in the stomach lining caused by elevated blood pressure in the portal vein.
Causes and Symptoms
Portal hypertension is commonly caused by liver cirrhosis and can lead to symptoms like ascites, varices, bleeding, and encephalopathy as a result of elevated blood pressure in the portal vein.
Clinical Manifestations of Portal Hypertension
Portal hypertension commonly leads to variceal bleeding and hepatic encephalopathy, causing severe complications in affected individuals.
Variceal Bleeding
Portal hypertension commonly results in variceal bleeding, a serious complication that can occur due to the development of enlarged veins in the esophagus and stomach, known as varices. These varices can rupture, leading to potentially life-threatening bleeding episodes.
Hepatic Encephalopathy
Hepatic encephalopathy is a potential complication of portal hypertension characterized by cognitive impairment and neurological symptoms due to liver dysfunction.
Cirrhosis can significantly impact portal hypertension, leading to complications like ascites, encephalopathy, variceal bleeding, and hepatorenal syndrome.

Impact of Cirrhosis on Portal Hypertension
Cirrhosis has a significant impact on portal hypertension, leading to complications like ascites, variceal bleeding, hepatic encephalopathy, and hepatorenal syndrome, resulting in substantial morbidity and mortality.
Prevention Strategies for Portal Hypertension
It is crucial to focus on lifestyle changes to prevent and manage portal hypertension, reducing the risk of complications.
Development and Progression
Complications of portal hypertension like ascites, variceal bleeding, hepatic encephalopathy, and hepatorenal syndrome contribute to substantial morbidity and mortality, emphasizing the need for effective management strategies.
Portal hypertension often develops as a consequence of liver damage, particularly in conditions like cirrhosis, leading to increased pressure in the portal vein and various complications.
Relationship with Liver Damage
Portal hypertension often develops as a consequence of liver damage, particularly in conditions like cirrhosis, leading to increased pressure in the portal vein and various complications.
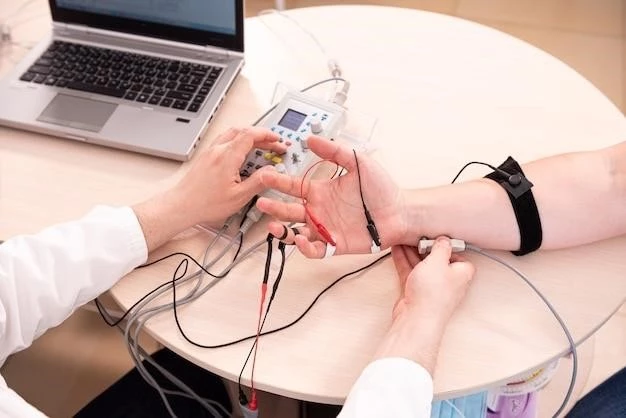
Noninvasive Techniques for Portal Hypertension Diagnosis
Portal hypertension can be diagnosed noninvasively using techniques like spleen stiffness measurement, which provides valuable insights into the severity of the condition without the need for invasive procedures.
Spleen Stiffness Measurement
Spleen stiffness measurement is a noninvasive technique used in diagnosing portal hypertension, providing valuable insights into the severity of the condition without the need for invasive procedures.
Researchers are continually developing new noninvasive diagnostic methods, such as spleen stiffness measurement, to enhance the diagnosis and monitoring of portal hypertension, providing more precise insights without invasive procedures.
Novel Diagnostic Approaches
Researchers are continually innovating new noninvasive diagnostic methods like spleen stiffness measurement to enhance the diagnosis and monitoring of portal hypertension, providing more precise insights without invasive procedures.
Prognosis and Long-term Outlook
Mortality rates and complications associated with portal hypertension highlight the importance of effective management strategies and continuous monitoring to improve long-term outcomes.
Mortality Rates and Complications
Understanding the mortality rates and complications associated with portal hypertension can provide insights into the long-term prognosis and guide effective management strategies to improve patient outcomes.