Hypogonadotropic Hypogonadism without Anosmia‚ X-Linked
I. Introduction to Hypogonadotropic Hypogonadism
Hypogonadotropic hypogonadism without anosmia‚ X-linked‚ is a rare genetic disorder characterized by a lack of puberty development in males due to reduced male hormone production. Unlike other forms of hypogonadotropic hypogonadism‚ the X-linked variant does not present with the typical symptom of anosmia (inability to smell).
This condition affects the normal functioning of the pituitary gland and disrupts the hormonal signals necessary for the onset of puberty and development of secondary sexual characteristics. Individuals with this disorder often experience delayed or absent puberty‚ reduced muscle mass‚ and underdeveloped genitalia.
Understanding the underlying causes‚ symptoms‚ diagnosis‚ and treatment of this condition is crucial in providing appropriate care and management for affected individuals. By delving into the genetic and physiological aspects of X-linked hypogonadotropic hypogonadism without anosmia‚ advancements in diagnosis and treatment can be further explored to improve outcomes for patients.
II. Understanding X-Linked Hypogonadotropic Hypogonadism
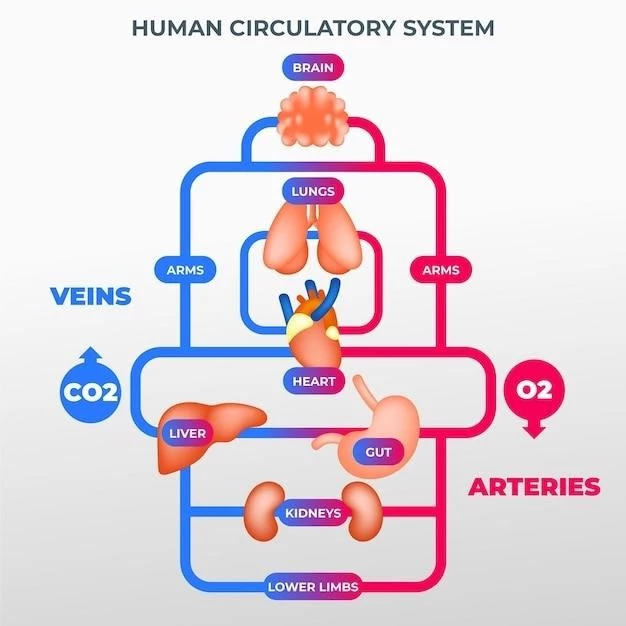
X-linked hypogonadotropic hypogonadism without anosmia is a genetic disorder linked to mutations in the Kallmann syndrome 1 (KAL1) gene located on the X chromosome. These mutations impair the normal production or function of the hormone gonadotropin-releasing hormone (GnRH) in the hypothalamus‚ leading to decreased signaling to the pituitary gland.
As a result‚ the pituitary gland fails to produce adequate levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH)‚ which are essential for normal puberty and reproductive function. Without proper stimulation from LH and FSH‚ the testes do not produce enough testosterone‚ impacting male sexual development and fertility.
Individuals with X-linked hypogonadotropic hypogonadism may exhibit a wide range of symptoms‚ including delayed puberty‚ small testes‚ micropenis‚ and infertility. While anosmia‚ the inability to smell‚ is a common feature in other forms of the condition‚ it is notably absent in the X-linked variant.
Understanding the genetic basis and hormonal disruptions in X-linked hypogonadotropic hypogonadism is key to developing targeted treatments that aim to restore hormone balance and promote normal puberty and reproductive function in affected individuals.
III. Causes and Mechanisms
X-linked hypogonadotropic hypogonadism without anosmia is primarily caused by genetic mutations in the Kallmann syndrome 1 (KAL1) gene on the X chromosome. These mutations disrupt the production or function of gonadotropin-releasing hormone (GnRH) in the hypothalamus‚ a crucial hormone involved in stimulating the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Without sufficient levels of LH and FSH‚ the testes do not receive the necessary signals to produce testosterone‚ resulting in impaired male sexual development and reproductive function. The inheritance pattern of X-linked hypogonadotropic hypogonadism without anosmia follows an X-linked recessive pattern‚ meaning the gene mutation is located on the X chromosome.
Genetic testing can identify mutations in the KAL1 gene‚ confirming the diagnosis of X-linked hypogonadotropic hypogonadism. Understanding the specific genetic alterations and their impact on hormonal pathways is crucial in elucidating the mechanisms underlying this disorder.
Research continues to explore the intricate mechanisms by which KAL1 gene mutations interfere with GnRH signaling and disrupt the hypothalamic-pituitary-gonadal axis. By unraveling these complex genetic and hormonal interactions‚ novel therapeutic targets may be identified to address the root cause of X-linked hypogonadotropic hypogonadism without anosmia.
IV. Symptoms and Clinical Presentation
X-linked hypogonadotropic hypogonadism without anosmia presents with a spectrum of clinical symptoms related to insufficient male hormone production and delayed puberty. Common manifestations include delayed onset or absence of puberty‚ small testes‚ reduced muscle mass‚ sparse body hair‚ and underdeveloped genitalia.
Individuals with this condition may experience infertility due to impaired sperm production resulting from the lack of testosterone stimulation. Additionally‚ affected males may exhibit micropenis‚ which can further impact their self-esteem and quality of life.
While anosmia is usually a hallmark feature of hypogonadotropic hypogonadism‚ it is notably absent in the X-linked variant. Diagnosis often involves thorough clinical evaluation‚ hormone testing‚ and genetic analysis to confirm the presence of KAL1 gene mutations.
Other less common symptoms of X-linked hypogonadotropic hypogonadism without anosmia may include decreased libido‚ erectile dysfunction‚ and reduced bone mineral density. Early recognition of these symptoms is crucial for timely intervention and management to support normal sexual development and reproductive health in affected individuals.
V. Diagnosis of X-Linked Hypogonadotropic Hypogonadism
Diagnosing X-linked hypogonadotropic hypogonadism without anosmia requires a comprehensive approach that combines clinical evaluation‚ hormone testing‚ and genetic analysis. Initial assessments typically involve a detailed medical history review to identify symptoms related to delayed puberty and male hormone deficiency.
Physical examination may reveal characteristic features such as small testes‚ micropenis‚ and underdeveloped secondary sexual characteristics. Laboratory tests measuring hormone levels‚ including luteinizing hormone (LH)‚ follicle-stimulating hormone (FSH)‚ and testosterone‚ can provide valuable insights into the hormonal imbalances associated with the condition.
Genetic testing plays a crucial role in confirming the diagnosis of X-linked hypogonadotropic hypogonadism by identifying mutations in the Kallmann syndrome 1 (KAL1) gene. This genetic analysis helps differentiate the X-linked form from other types of hypogonadotropic hypogonadism and guides appropriate management strategies.
In some cases‚ advanced imaging studies‚ such as magnetic resonance imaging (MRI) of the brain‚ may be recommended to assess the structure of the hypothalamus and pituitary gland. These imaging modalities can help rule out other underlying causes of hypogonadotropic hypogonadism and provide additional diagnostic information.
VI. Treatment Approaches
The management of X-linked hypogonadotropic hypogonadism without anosmia aims to address the underlying hormonal deficiencies and support normal male development and reproductive function. Testosterone replacement therapy is a cornerstone of treatment to supplement low testosterone levels and promote secondary sexual characteristics.
Testosterone can be administered through various means‚ including intramuscular injections‚ transdermal patches‚ or topical gels. Regular monitoring of hormone levels is essential to ensure that testosterone concentrations are within the therapeutic range and to adjust treatment as needed.
In cases where fertility is desired‚ gonadotropin therapy may be considered to stimulate sperm production. This approach involves the administration of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) to support testicular function and enhance fertility potential.
Psychological support and counseling play a vital role in helping individuals cope with the emotional and psychological impact of delayed puberty and fertility issues associated with X-linked hypogonadotropic hypogonadism. Educating patients and their families about the condition and available treatment options is key to fostering informed decision-making and optimal outcomes.
Ongoing monitoring by healthcare providers‚ including endocrinologists and reproductive specialists‚ is crucial to assess treatment response‚ manage potential side effects‚ and address any emerging concerns related to the condition. Collaborative care involving a multidisciplinary team can provide comprehensive support for individuals with X-linked hypogonadotropic hypogonadism throughout their treatment journey;
VII. Management and Long-Term Outlook
The long-term management of X-linked hypogonadotropic hypogonadism without anosmia involves regular monitoring of hormone levels‚ treatment adjustment as needed‚ and addressing any specific health concerns that may arise. Close collaboration between healthcare providers and individuals affected by the condition is essential for optimizing outcomes and quality of life.
Adherence to testosterone replacement therapy and gonadotropin treatment‚ if indicated‚ is crucial to maintaining appropriate hormone levels and supporting normal sexual development. Monitoring for potential side effects of testosterone therapy‚ such as acne‚ mood changes‚ and erythrocytosis‚ is important to minimize risks and ensure treatment efficacy.
Individuals with X-linked hypogonadotropic hypogonadism may benefit from ongoing counseling and psychological support to address any emotional challenges related to delayed puberty‚ fertility concerns‚ or body image issues. Education about the condition‚ treatment options‚ and reproductive implications can empower patients to make informed decisions about their care.
Regular follow-up appointments with endocrinologists and reproductive specialists allow for comprehensive evaluation of treatment response‚ adjustments to therapy‚ and addressing any emerging needs or questions. Monitoring bone health‚ cardiovascular risk factors‚ and fertility parameters is integral to overall health management in individuals with this condition.
With appropriate management and support‚ individuals with X-linked hypogonadotropic hypogonadism can lead fulfilling lives and achieve milestones in their personal and reproductive health. By proactively addressing hormonal deficiencies and understanding the long-term implications of the condition‚ healthcare providers can help patients navigate their journey with confidence and resilience.
VIII. Research and Advancements in Treatment
Ongoing research in X-linked hypogonadotropic hypogonadism without anosmia is focused on advancing treatment options and understanding the underlying genetic and hormonal mechanisms of the condition. Recent studies have identified novel gene mutations associated with the disorder‚ shedding light on potential targets for therapeutic interventions.
Advancements in gene therapy and gene editing technologies offer promising avenues for correcting genetic abnormalities in conditions like X-linked hypogonadotropic hypogonadism. By developing targeted approaches to restore normal gene function‚ researchers aim to address the root cause of hormonal imbalances and improve treatment outcomes.
Clinical trials investigating the efficacy and safety of new treatment modalities‚ such as GnRH analogs‚ selective estrogen receptor modulators‚ and gonadotropin therapy‚ are underway to expand the armamentarium of options available for individuals with X-linked hypogonadotropic hypogonadism. These trials seek to optimize treatment regimens‚ enhance fertility outcomes‚ and minimize side effects.
Moreover‚ research efforts are focused on elucidating the long-term implications of X-linked hypogonadotropic hypogonadism on bone health‚ cardiovascular function‚ and metabolic parameters. By understanding the broader health implications of the condition‚ clinicians can provide comprehensive care that addresses both hormonal deficiencies and related comorbidities.
Collaboration between basic scientists‚ clinical researchers‚ and healthcare providers is essential in driving innovation and translating scientific discoveries into clinical practice. Through multidisciplinary approaches and the integration of cutting-edge technologies‚ the field of X-linked hypogonadotropic hypogonadism research continues to evolve‚ offering hope for improved treatments and better outcomes for individuals affected by this rare genetic disorder.
IX. Psychological and Social Impacts
X-linked hypogonadotropic hypogonadism without anosmia can have profound psychological and social impacts on affected individuals. The delayed onset of puberty‚ physical characteristics like small testes and micropenis‚ and fertility issues associated with the condition can significantly affect self-esteem‚ body image‚ and mental well-being.
Adolescents and adults with X-linked hypogonadotropic hypogonadism may experience feelings of inadequacy‚ isolation‚ and depression due to challenges in sexual development and reproductive health. These psychological impacts can extend to interpersonal relationships‚ social interactions‚ and overall quality of life.
Counseling and psychotherapy play a crucial role in supporting individuals with X-linked hypogonadotropic hypogonadism‚ helping them navigate the emotional complexities of living with a rare genetic disorder. Psychosocial support can assist in coping with feelings of shame‚ stigma‚ and uncertainty surrounding fertility and sexual health.
Educating patients‚ families‚ and caregivers about the psychological aspects of the condition is essential in promoting understanding‚ empathy‚ and effective communication. Addressing mental health concerns proactively and providing resources for emotional support can empower individuals to seek help and engage in self-care strategies.
Furthermore‚ raising awareness about X-linked hypogonadotropic hypogonadism within the medical community and society at large can reduce misunderstandings and promote acceptance and inclusion. By fostering a supportive environment that recognizes the unique challenges faced by individuals with this rare disorder‚ we can work towards enhancing overall well-being and resilience in affected individuals.
X. Lifestyle Modifications and Self-Care
Individuals with X-linked hypogonadotropic hypogonadism can benefit from certain lifestyle modifications and self-care practices to support their overall well-being and manage the impact of the condition on their daily lives. Maintaining a healthy lifestyle through regular physical activity‚ a nutritious diet‚ and adequate sleep is essential for optimizing physical and mental health.
Regular exercise‚ including strength training and cardiovascular activities‚ can help promote muscle strength‚ bone density‚ and overall fitness in individuals with X-linked hypogonadotropic hypogonadism. Consultation with healthcare providers or physical therapists to develop personalized exercise regimens is recommended to ensure safety and efficacy.
A balanced diet rich in essential nutrients‚ vitamins‚ and minerals is pivotal for supporting hormonal balance‚ bone health‚ and energy levels. Incorporating foods high in protein‚ fiber‚ healthy fats‚ and antioxidants can contribute to overall well-being and may help mitigate some of the metabolic effects associated with the condition.
Self-care practices such as stress management techniques‚ mindfulness‚ and relaxation exercises can be beneficial in coping with the emotional challenges and psychological impacts of X-linked hypogonadotropic hypogonadism. Seeking social support from family‚ friends‚ or support groups can also provide emotional resilience and foster a sense of community.
Regular medical check-ups‚ adherence to prescribed treatment regimens‚ and open communication with healthcare providers are essential components of self-care for individuals with X-linked hypogonadotropic hypogonadism. By taking an active role in their health management and well-being‚ individuals can empower themselves to navigate the complexities of living with a rare genetic disorder.
XI. Family Planning and Genetic Counseling
Family planning and genetic counseling play pivotal roles in the management of X-linked hypogonadotropic hypogonadism without anosmia‚ as they encompass crucial aspects of reproductive health and hereditary risk assessment. Individuals diagnosed with the condition should receive comprehensive genetic counseling to understand the inheritance pattern‚ risks of passing the gene mutation to offspring‚ and available reproductive options.
Genetic counselors can provide personalized information about the genetic basis of X-linked hypogonadotropic hypogonadism‚ discuss implications for family members‚ and guide individuals in making informed decisions about family planning. Carrier testing and prenatal genetic screening may be considered to assess the risk of transmission and plan for future pregnancies.
For couples affected by X-linked hypogonadotropic hypogonadism‚ assisted reproductive technologies such as in vitro fertilization (IVF) with preimplantation genetic testing can offer options for selecting embryos without the genetic mutation before pregnancy. This approach can help reduce the likelihood of passing the disorder to offspring.
Open and honest communication between partners‚ as well as involvement of healthcare providers specializing in reproductive genetics‚ can facilitate shared decision-making and support in navigating complex familial and genetic considerations. Embracing the support of a multidisciplinary team that includes genetic counselors‚ endocrinologists‚ and fertility specialists is crucial in addressing family planning needs and promoting informed choices.
By integrating family planning discussions and genetic counseling into the care of individuals with X-linked hypogonadotropic hypogonadism‚ healthcare providers can empower patients and their families to make decisions that align with their values‚ preferences‚ and reproductive goals. Ensuring access to comprehensive reproductive health services and education is paramount in optimizing reproductive outcomes and promoting genetic well-being within affected families.
XII. Conclusion
In conclusion‚ X-linked hypogonadotropic hypogonadism without anosmia is a rare genetic disorder that presents unique challenges in male hormone production‚ puberty development‚ and reproductive health. Understanding the genetic basis‚ hormonal disruptions‚ and clinical manifestations of this condition is essential for accurate diagnosis and effective management.
Advancements in research and treatment have contributed to expanding therapeutic options‚ including testosterone replacement therapy‚ gonadotropin stimulation‚ and emerging genetic interventions. By leveraging multidisciplinary approaches and staying abreast of scientific developments‚ healthcare providers can offer comprehensive care that addresses the physical‚ hormonal‚ psychological‚ and social aspects of X-linked hypogonadotropic hypogonadism.
Psychological support‚ lifestyle modifications‚ and genetic counseling play integral roles in supporting individuals with the condition and their families. Empowering patients through education‚ counseling‚ and self-care strategies can enhance well-being and quality of life while navigating the complexities of a genetic disorder that impacts multiple facets of health and reproduction.
Moving forward‚ continued research efforts‚ advancements in genetic technologies‚ and collaborative care models hold promise for further improving outcomes and addressing the long-term implications of X-linked hypogonadotropic hypogonadism without anosmia. By advocating for holistic care‚ promoting awareness‚ and fostering a supportive environment‚ we can enhance the resilience and well-being of individuals affected by this rare genetic disorder.