Hypokalemic Periodic Paralysis Type 1
Hypokalemic Periodic Paralysis Type 1 is a rare genetic disorder that affects muscle function due to a mutation in ion channels related to the sodium-potassium pump․ It leads to periodic attacks of muscle weakness or paralysis, triggered by factors like stress or certain foods․ Understanding potassium’s role in muscle contractions is crucial in managing this condition․ Keeping a close watch on calcium levels is important for nerve cell function and overall health․
Introduction to Hypokalemic Periodic Paralysis Type 1
Hypokalemic Periodic Paralysis Type 1 is a rare neuromuscular disorder characterized by episodes of muscle weakness or paralysis․ It is caused by a genetic mutation affecting ion channels responsible for maintaining the balance of potassium levels in muscle cells․ This balance is crucial for proper muscle function, and any disruption can lead to debilitating symptoms․
Individuals with this condition may experience periodic attacks where they suddenly lose strength in their muscles, often triggered by factors like stress, certain medications, or a high-carb meal․ These attacks can be frightening and debilitating, affecting daily activities and quality of life․ Understanding the underlying mechanisms of this disorder is essential for effective management․
During an attack, muscle stiffness, cramps, and even paralysis can occur․ This happens because low potassium levels, known as hypokalemia, impair the ability of muscles to contract properly․ The sodium-potassium pump, a vital mechanism in muscle cells, is disrupted by the genetic mutation seen in Type 1 Hypokalemic Periodic Paralysis․
These attacks can range from mild weakness to severe paralysis, lasting from a few hours to several days in some cases․ The unpredictability of when an attack may strike adds to the challenges faced by individuals with this condition․ Seeking a proper diagnosis and understanding potential trigger factors can help in managing and preventing these episodes․
Living with Hypokalemic Periodic Paralysis Type 1 requires careful monitoring of potassium levels and working closely with healthcare providers to develop a personalized treatment plan․ By taking proactive steps to maintain potassium balance and avoid triggers, individuals can minimize the impact of the disorder on their daily lives․
Understanding Potassium and its Role in the Body
Potassium is a vital mineral that plays a crucial role in various bodily functions, particularly in muscle contractions and nerve cell activity․ In the context of Hypokalemic Periodic Paralysis Type 1, potassium levels are of utmost importance due to their impact on muscle function․
Within muscle cells, potassium is involved in regulating the electrical impulses that control muscle contractions․ When potassium levels are too low, as seen in hypokalemia, the ability of muscles to contract effectively is impaired․ This can lead to symptoms such as muscle weakness, cramps, and even paralysis․
The balance between potassium and sodium is essential for maintaining proper muscle function․ Potassium is mainly found inside cells, while sodium is more prevalent outside cells․ The sodium-potassium pump, a critical mechanism in muscle cells, helps maintain this balance by pumping sodium out of the cell and potassium in․
In individuals with Hypokalemic Periodic Paralysis Type 1, a genetic mutation affects this pump’s function, disrupting the balance of potassium and sodium․ This imbalance can trigger periodic attacks of muscle weakness or paralysis, highlighting the importance of monitoring potassium levels․
It is essential for individuals with this condition to be aware of their potassium intake and ensure they are getting an adequate amount through their diet․ Foods rich in potassium include bananas, potatoes, spinach, and avocados․ However, dietary changes should be made in consultation with a healthcare provider to prevent sudden fluctuations in potassium levels․
By understanding the role of potassium in muscle function and nerve cell activity, individuals with Hypokalemic Periodic Paralysis Type 1 can take proactive steps to manage their condition effectively․ Regular monitoring of potassium levels and adopting a potassium-rich diet can help support muscle health and reduce the frequency and severity of attacks․
Genetic Mutation and Sodium-Potassium Pump
In the context of Hypokalemic Periodic Paralysis Type 1, a genetic mutation affects the sodium-potassium pump, a critical mechanism responsible for maintaining the balance of potassium and sodium levels in muscle cells․ This mutation disrupts the pump’s function, leading to abnormal potassium levels within the cells․
The sodium-potassium pump is essential for regulating the electrical charge across cell membranes, particularly in muscle cells․ It works by actively transporting sodium ions out of the cell and potassium ions into the cell․ This process is crucial for muscle contractions, nerve cell communication, and overall cellular function․
Individuals with Hypokalemic Periodic Paralysis Type 1 inherit a genetic mutation that impacts the sodium-potassium pump’s ability to maintain the proper balance of ions․ As a result٫ muscle cells may have lower-than-normal levels of potassium٫ leading to episodes of muscle weakness or paralysis during attacks․
The disruption of the sodium-potassium pump can also affect nerve cell function, as these cells rely on the pump to maintain the appropriate ion concentrations for communication․ Abnormal potassium levels can influence the generation and transmission of electrical impulses along nerve cells, contributing to the symptoms experienced in this disorder․
Understanding the genetic basis of Hypokalemic Periodic Paralysis Type 1 and its impact on the sodium-potassium pump is crucial for managing the condition effectively․ Genetic testing can help confirm the presence of the mutation and guide treatment decisions to alleviate symptoms and prevent complications․
By working closely with healthcare providers to understand the implications of the genetic mutation and its effects on the sodium-potassium pump, individuals with this condition can better navigate their care and make informed choices regarding treatment options․ Monitoring potassium levels and addressing any disruptions in the pump’s function are key components of managing Hypokalemic Periodic Paralysis Type 1․
Symptoms of Hypokalemic Periodic Paralysis Type 1
Hypokalemic Periodic Paralysis Type 1 is characterized by episodes of muscle weakness or paralysis that occur periodically․ These episodes can vary in severity and duration, impacting the individual’s ability to move and perform daily activities․ Understanding the symptoms associated with this condition is crucial for timely recognition and appropriate management․
During an attack of Hypokalemic Periodic Paralysis Type 1, individuals may experience muscle stiffness, cramps, and a sensation of muscle weakness․ These symptoms typically affect the limbs but can also involve muscles in the face, neck, and trunk․ The weakness can range from mild to severe and may progress to partial or complete paralysis․
One of the hallmark features of this condition is the episodic nature of the attacks․ These episodes can be triggered by various factors, such as stress, certain medications, or foods high in carbohydrates; Identifying and avoiding these trigger factors can help reduce the frequency and intensity of attacks in individuals with Hypokalemic Periodic Paralysis Type 1․
Individuals may also experience muscle cramps, which can be painful and contribute to the overall discomfort during an attack․ These cramps are often linked to the abnormal potassium levels in muscle cells, leading to changes in muscle function and contractions․ Managing potassium balance through dietary adjustments and medication can help alleviate cramping symptoms․
In some cases, individuals with this condition may also notice changes in sensation, such as tingling or numbness in the affected muscles․ These sensory changes can accompany muscle weakness and provide additional clues to the onset of an attack․ Recognizing these sensory symptoms is important for early intervention and prevention of more severe paralysis․
Being aware of the typical symptoms associated with Hypokalemic Periodic Paralysis Type 1 allows individuals and healthcare providers to develop a comprehensive management plan tailored to the individual’s needs․ By closely monitoring symptom patterns and addressing triggers promptly, the impact of this condition on daily life can be minimized, improving overall quality of life․
Muscle Contractions and Hypokalemia
Muscle contractions are essential for movement and various bodily functions, relying on the intricate balance of ions, including potassium, within muscle cells․ In the context of Hypokalemic Periodic Paralysis Type 1, disruptions in potassium levels, known as hypokalemia, can significantly impact muscle contractions and lead to debilitating symptoms․
Potassium plays a crucial role in regulating the electrical impulses that trigger muscle contractions․ When potassium levels are low, as seen in hypokalemia, the ability of muscles to contract effectively is compromised․ This can manifest as muscle weakness, stiffness, cramps, and in severe cases, paralysis․
Individuals with Hypokalemic Periodic Paralysis Type 1 may experience episodes of muscle weakness or paralysis due to the abnormal potassium levels in muscle cells․ These episodes are often unpredictable and can be triggered by factors like stress, certain medications, or high-carbohydrate meals․
During an attack of this condition, the disrupted potassium balance interferes with the muscle fibers’ ability to contract and relax properly․ This results in the characteristic symptoms of muscle weakness and may progress to more severe paralysis, affecting mobility and day-to-day activities․
It is important for individuals with Hypokalemic Periodic Paralysis Type 1 to understand the relationship between muscle contractions and hypokalemia to effectively manage their condition․ By working closely with healthcare providers, monitoring potassium levels, and identifying trigger factors that exacerbate symptoms, individuals can take proactive steps to prevent and mitigate attacks․
Addressing hypokalemia through dietary modifications, potassium supplements, and avoiding triggers known to precipitate attacks can help in stabilizing potassium levels and supporting muscle function․ By optimizing potassium balance and promoting healthy muscle contractions, individuals with this condition can enhance their quality of life and overall well-being․
Trigger Factors for Hypokalemic Periodic Paralysis Attacks
Understanding the trigger factors for Hypokalemic Periodic Paralysis attacks is crucial for individuals with this condition to effectively manage and prevent episodes of muscle weakness or paralysis․ Various factors can precipitate an attack, and being aware of these triggers empowers individuals to take proactive steps in their care․
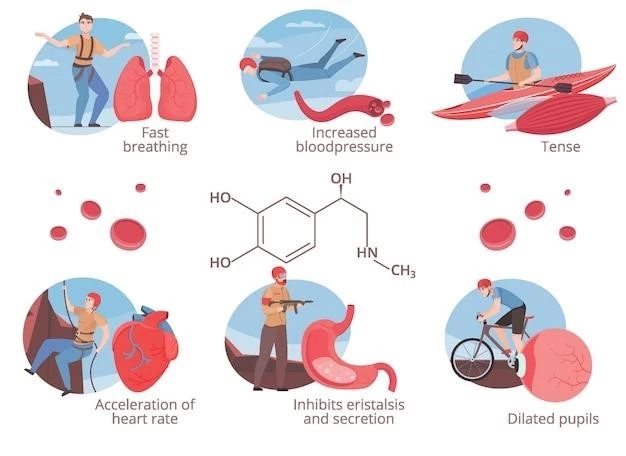
Stress is a common trigger for Hypokalemic Periodic Paralysis attacks, as emotional or physical stress can disrupt the delicate balance of potassium levels in muscle cells․ Managing stress through relaxation techniques, mindfulness, and stress-reducing activities can help minimize the risk of an attack․
Certain medications can also contribute to the onset of an attack in individuals with this condition․ It is essential for healthcare providers to be aware of all medications, including over-the-counter drugs and supplements, to assess their potential impact on potassium levels and muscle function․
Dietary factors play a significant role in triggering episodes of muscle weakness or paralysis in individuals with Hypokalemic Periodic Paralysis Type 1․ Foods high in carbohydrates, especially fast-absorbing sugars, can lead to fluctuations in blood sugar levels and subsequently affect potassium balance․
Changes in temperature, particularly exposure to extreme cold, can also act as a trigger for attacks in some individuals․ Maintaining a comfortable environment and dressing appropriately for the weather can help prevent temperature-related triggers from inducing episodes of muscle weakness․
In addition to external triggers, hormonal changes, such as those during menstrual cycles or pregnancy, can influence the onset of attacks in individuals with this condition․ Understanding how hormones impact potassium regulation and muscle function can aid in managing the condition during these times;
By identifying and avoiding trigger factors specific to their circumstances, individuals with Hypokalemic Periodic Paralysis Type 1 can better control the frequency and severity of attacks․ Working collaboratively with healthcare providers to develop a comprehensive plan that addresses trigger avoidance and symptom management is essential for optimizing quality of life․
Diagnosis and Treatment of Type 1 Hypokalemic Periodic Paralysis
Diagnosing and treating Type 1 Hypokalemic Periodic Paralysis requires a comprehensive approach to address the genetic mutation affecting ion channels and the sodium-potassium pump․ Healthcare providers use various methods to confirm the diagnosis and develop a personalized treatment plan tailored to each individual’s needs․
Genetic testing plays a crucial role in diagnosing Type 1 Hypokalemic Periodic Paralysis․ By identifying the specific genetic mutation responsible for the condition, healthcare providers can confirm the diagnosis and assess the likelihood of passing the mutation to future generations․
Electromyography (EMG) and nerve conduction studies are commonly used to evaluate muscle and nerve function in individuals with suspected Hypokalemic Periodic Paralysis․ These tests can help assess the extent of muscle weakness or paralysis during an attack and guide treatment decisions․
Monitoring potassium levels through blood tests is essential for individuals with this condition․ Regular assessment of potassium levels helps healthcare providers adjust treatment strategies, such as potassium supplements or dietary modifications, to maintain optimal levels and prevent attacks․
Treatment for Type 1 Hypokalemic Periodic Paralysis focuses on managing symptoms, preventing attacks, and improving overall muscle function․ Potassium supplements are often prescribed to help stabilize potassium levels and support proper muscle contractions․
Individuals with this condition are advised to work closely with healthcare providers to develop a personalized treatment plan that addresses their specific needs and circumstances․ Physical therapy may be recommended to help maintain muscle strength and mobility during and between attacks․
Avoiding trigger factors, such as stress, certain medications, and high-carb foods, is an essential part of managing Type 1 Hypokalemic Periodic Paralysis․ By identifying and addressing these triggers, individuals can reduce the frequency and severity of attacks and improve their quality of life․
Regular follow-up appointments with healthcare providers are important for monitoring treatment effectiveness, adjusting interventions as needed, and addressing any concerns or new symptoms that may arise․ By actively participating in their care, individuals with Type 1 Hypokalemic Periodic Paralysis can achieve better symptom control and overall well-being․
Importance of Monitoring Calcium Levels
While potassium levels play a central role in Hypokalemic Periodic Paralysis Type 1٫ monitoring calcium levels is also crucial for maintaining overall health and nerve cell function․ Calcium is vital for numerous physiological processes٫ including muscle contractions٫ nerve signaling٫ and bone health․
In individuals with Hypokalemic Periodic Paralysis Type 1, disruptions in potassium levels can indirectly impact calcium balance and utilization within the body․ Fluctuations in calcium levels can influence muscle function, nerve cell communication, and the severity of symptoms experienced during attacks․
Calcium is essential for the release of neurotransmitters involved in muscle contractions and nerve impulses․ Changes in calcium concentrations can affect the ability of nerve cells to transmit signals efficiently, leading to abnormalities in muscle function and coordination․
Monitoring calcium levels through blood tests is an integral part of managing Hypokalemic Periodic Paralysis Type 1․ Healthcare providers use these tests to assess calcium status, identify any imbalances, and ensure that calcium intake from diet and supplements is sufficient for optimal health․
Individuals with this condition are encouraged to consume calcium-rich foods, such as dairy products, leafy green vegetables, and fortified foods, to support bone health and muscle function․ Adequate calcium intake can help mitigate the impact of abnormal potassium levels on muscle contractions․
In some cases, calcium supplements may be recommended to maintain adequate levels in the body, especially if dietary sources are insufficient․ However, calcium supplementation should be managed carefully under the guidance of healthcare providers to prevent interactions with other medications and potential complications․
By monitoring and optimizing calcium levels alongside potassium levels, individuals with Hypokalemic Periodic Paralysis Type 1 can support overall muscle and nerve function٫ reduce the risk of complications٫ and enhance their quality of life․ Regular communication with healthcare providers is essential to ensure a comprehensive approach to managing this complex neuromuscular disorder․