Understanding Gangliosidosis (Type 2) ⎼ GM2 Disease
Overview of Gangliosidosis (GM2)
Gangliosidosis is a type of lysosomal storage disorder characterized by the accumulation of gangliosides in cells. GM2 gangliosidosis refers specifically to the group of diseases caused by a deficiency of the enzyme hexosaminidase A٫ leading to the buildup of GM2 gangliosides.
There are two main forms of GM2 disease⁚ Tay-Sachs disease and Sandhoff disease. Both are infantile neurodegenerative disorders that progressively affect neurological function due to the mutation in the HEXA gene encoding the hexosaminidase A enzyme.
Individuals with GM2 gangliosidosis experience a spectrum of symptoms, including developmental delays, muscle weakness, seizures, vision and hearing problems, and ultimately, a decline in mental abilities. The neurological decline is relentless and irreversible, often leading to premature death in early childhood.
Diagnosis of GM2 disease involves a combination of clinical symptoms, enzyme activity assays, and genetic testing. While there is currently no cure for GM2 gangliosidosis, treatment aims to manage symptoms and improve quality of life through supportive care, physical therapy, and symptom-specific interventions.
Genetic counseling is essential for families affected by GM2 disease, as it helps individuals understand the inheritance pattern and risks associated with the condition. Family planning options such as prenatal testing and preimplantation genetic diagnosis can assist in making informed decisions about future pregnancies.
Ongoing research in the field of lysosomal storage disorders offers hope for new therapeutic approaches, including enzyme replacement therapy, substrate reduction therapy, and gene therapy, which may improve outcomes for individuals with GM2 gangliosidosis in the future.
Types of GM2 Disease
GM2 gangliosidosis encompasses two main types of diseases⁚ Tay-Sachs disease and Sandhoff disease. These conditions are both classified under the umbrella of GM2 due to their shared pathophysiology involving the accumulation of GM2 gangliosides in cells.
Tay-Sachs Disease⁚ Tay-Sachs disease is a rare autosomal recessive disorder caused by a deficiency of the hexosaminidase A enzyme. The mutation in the HEXA gene leads to the progressive accumulation of GM2 gangliosides in the lysosomes of nerve cells٫ resulting in the characteristic neurodegenerative symptoms associated with the disease.
Sandhoff Disease⁚ Sandhoff disease is another form of GM2 gangliosidosis caused by a deficiency of both hexosaminidase A and hexosaminidase B enzymes due to mutations in the HEXB gene. This results in the buildup of not only GM2 gangliosides but also globosides, leading to a more severe and rapid progression of neurological symptoms compared to Tay-Sachs disease.
While both Tay-Sachs and Sandhoff diseases share similarities in their underlying cause and manifestation, they may present with varying degrees of severity and age of onset. Genetic testing is crucial for accurately diagnosing the specific type of GM2 disease and informing appropriate management strategies for affected individuals.
Understanding the distinct characteristics of Tay-Sachs and Sandhoff diseases is essential for healthcare providers, researchers, and families impacted by GM2 gangliosidosis. By differentiating between these two types of GM2 disease, interventions and support can be tailored to meet the specific needs of each patient and family affected by these devastating conditions.
Understanding the Pathophysiology
The pathophysiology of GM2 gangliosidosis, including Tay-Sachs and Sandhoff diseases, revolves around the deficiency of the hexosaminidase A enzyme, crucial for the breakdown of GM2 gangliosides. Without sufficient enzyme activity, these lipid molecules accumulate within lysosomes, disrupting cellular function and leading to neurodegeneration.
GM2 gangliosides are predominantly found in the nervous system, particularly in neuronal membranes. Their accumulation impairs lysosomal function and disrupts vital cellular processes, contributing to the progressive deterioration seen in individuals with GM2 disease.
The HEXA gene mutation in Tay-Sachs disease results in the absence or reduced activity of hexosaminidase A, leading to the buildup of GM2 gangliosides in neurons. Similarly, in Sandhoff disease, mutations in the HEXB gene cause deficiencies in both hexosaminidase A and B enzymes, resulting in the accumulation of a broader spectrum of glycolipids.
As GM2 gangliosides accumulate٫ they interfere with cellular signaling٫ membrane stability٫ and neuronal function٫ ultimately leading to neuronal death and the debilitating neurological symptoms characteristic of GM2 gangliosidosis. The lipid-laden lysosomes swell٫ impairing cell viability and contributing to the pathology of the disease.
Understanding the precise mechanisms underlying the pathophysiology of GM2 gangliosidosis is crucial for developing targeted therapies aimed at restoring enzyme function, reducing ganglioside accumulation, and preserving neuronal health. Research efforts focused on elucidating the molecular pathways disrupted by GM2 disease offer promising avenues for potential interventions to alleviate the devastating impact of these neurodegenerative disorders.
Hexosaminidase A Enzyme Deficiency
Hexosaminidase A enzyme deficiency is the primary defect underlying GM2 gangliosidosis, specifically Tay-Sachs and Sandhoff diseases; This enzyme plays a crucial role in breaking down GM2 gangliosides within lysosomes, the cellular compartments responsible for waste disposal.
The deficiency of hexosaminidase A results from genetic mutations affecting the HEXA gene in Tay-Sachs disease and both the HEXA and HEXB genes in Sandhoff disease. These mutations lead to impaired or absent enzyme activity, causing the toxic accumulation of GM2 gangliosides and other glycolipids in cells٫ particularly neurons.
Hexosaminidase A deficiency disrupts the normal degradation pathway of GM2 gangliosides٫ leading to their storage within lysosomes and interfering with essential cellular processes. Without proper enzymatic activity٫ the lipids continue to amass٫ causing cellular dysfunction٫ lysosomal swelling٫ and ultimately٫ neuronal death.
The loss of hexosaminidase A function in GM2 gangliosidosis results in a cascade of cellular events that culminate in the progressive neurodegeneration seen in affected individuals. The relentless buildup of gangliosides in neurons contributes to the wide range of neurological symptoms characteristic of these disorders.
Research efforts focused on understanding the mechanisms of hexosaminidase A deficiency and its consequences on cellular function are vital for developing targeted therapies to restore enzyme activity, reduce ganglioside accumulation, and mitigate the debilitating effects of GM2 gangliosidosis on the nervous system.
Symptoms and Progression
Individuals with GM2 gangliosidosis٫ such as Tay-Sachs and Sandhoff diseases٫ exhibit a spectrum of symptoms that worsen over time due to the progressive nature of these neurodegenerative disorders. The onset and severity of symptoms can vary depending on the specific genetic mutations and type of GM2 disease.
Early signs of GM2 gangliosidosis often manifest in infancy or early childhood and may include developmental delays, muscle weakness, exaggerated startle response, loss of motor skills, seizures, and vision or hearing impairment. As the diseases advance, affected individuals experience a decline in cognitive function, worsening motor abilities, and the loss of previously acquired skills.
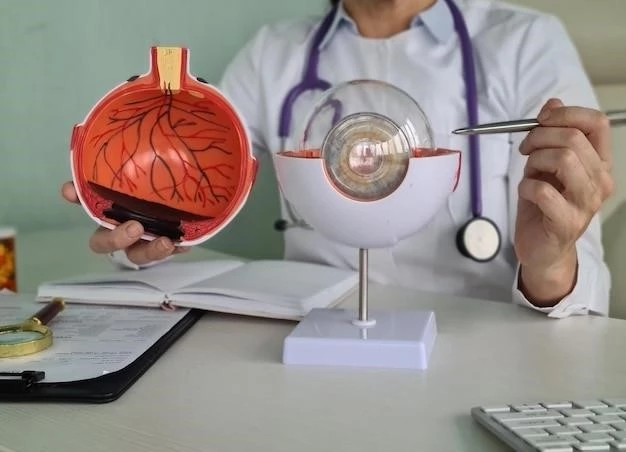
Neurological symptoms of GM2 disease progressively worsen٫ leading to spasticity٫ seizures٫ difficulty swallowing٫ and respiratory complications. Individuals may also develop cherry-red spots in the eyes٫ a characteristic feature of these disorders. The relentless neurodegeneration ultimately results in profound intellectual disability and premature death in many cases.
The progression of Tay-Sachs and Sandhoff diseases is rapid, with affected individuals experiencing a rapid decline in neurological function and quality of life. The severe and irreversible nature of these disorders poses significant challenges for patients, families, and healthcare providers, requiring comprehensive support and symptom management.
Understanding the evolving symptoms and progression of GM2 gangliosidosis is essential for early detection, accurate diagnosis, and timely intervention to improve the quality of life for affected individuals. Ongoing research aimed at unraveling the mechanisms driving disease progression offers hope for developing targeted therapies to slow the neurodegenerative course of these devastating disorders.
Diagnosis of GM2 Disease
Diagnosing GM2 gangliosidosis involves a comprehensive approach that integrates clinical evaluation, enzymatic assays, and genetic testing to confirm the presence of Tay-Sachs or Sandhoff disease. Early and accurate diagnosis is crucial for initiating appropriate management strategies and providing supportive care to individuals affected by these devastating neurodegenerative disorders.
Clinical assessment plays a key role in identifying the initial symptoms and signs of GM2 disease, such as developmental delays, muscle weakness, and neurological abnormalities. Healthcare providers may conduct physical exams, review medical history, and perform neurological assessments to evaluate the progression of the disease and plan for further diagnostic investigations.
Enzymatic assays are commonly used to measure the activity of hexosaminidase A enzyme to identify deficiencies indicative of GM2 gangliosidosis. Reduced enzyme activity levels in blood samples or other tissues provide valuable insights into the underlying enzymatic defects associated with Tay-Sachs and Sandhoff diseases.
Genetic testing is essential for confirming the diagnosis of GM2 disease by identifying specific mutations in the HEXA or HEXB genes responsible for encoding hexosaminidase A and B enzymes, respectively. Molecular analysis can pinpoint the genetic alterations that lead to enzyme deficiency and GM2 ganglioside accumulation, aiding in disease confirmation and family counseling.
Advanced diagnostic techniques, including next-generation sequencing and prenatal testing, offer additional insights into the genetic basis of GM2 gangliosidosis, enabling early detection of the disease in at-risk individuals and providing information for family planning purposes. Collaborative efforts between healthcare providers, genetic counselors, and researchers are crucial for facilitating the accurate and timely diagnosis of GM2 disease.
Treatment and Management
Currently, there is no cure for GM2 gangliosidosis٫ including Tay-Sachs and Sandhoff diseases. Treatment strategies focus on managing symptoms٫ providing supportive care٫ and enhancing the quality of life for individuals affected by these relentless neurodegenerative disorders.
Supportive care plays a crucial role in addressing the diverse needs of individuals with GM2 disease. This may include physical therapy to improve mobility and reduce muscle stiffness, occupational therapy to support daily activities, and speech therapy to aid in communication as neurological functions decline.
Seizure management is essential in individuals with GM2 gangliosidosis٫ and antiepileptic medications may be prescribed to control seizures and improve overall quality of life. Nutritional support٫ including feeding tubes if necessary٫ ensures adequate nutrient intake and prevents complications related to swallowing difficulties.
Palliative care focuses on enhancing comfort, managing pain, and addressing end-of-life care considerations for individuals with advanced GM2 gangliosidosis. Multidisciplinary care teams, including physicians, nurses, social workers, and palliative care specialists, collaborate to provide holistic support for patients and their families.
While specific treatments for reversing the neurodegenerative process in GM2 disease are lacking٫ ongoing research explores potential therapeutic avenues٫ including enzyme replacement therapy٫ substrate reduction therapy٫ and gene therapy. These innovative approaches aim to address the underlying enzymatic deficiencies and reduce ganglioside accumulation in affected cells.
Emotional and psychological support for individuals and families impacted by GM2 gangliosidosis is essential throughout the disease journey. Counseling services٫ caregiver support groups٫ and access to community resources can facilitate coping mechanisms٫ improve quality of life٫ and foster a sense of resilience in the face of these challenging conditions.
By emphasizing comprehensive treatment and management strategies that encompass medical, social, and emotional aspects, healthcare providers can enhance the well-being of individuals living with GM2 gangliosidosis and support their families through the complexities of these progressive neurodegenerative disorders.
Genetic Counseling and Family Planning
Genetic counseling plays a crucial role in the management of GM2 gangliosidosis, providing individuals and families with essential information about the genetic basis of Tay-Sachs and Sandhoff diseases, inheritance patterns, and available testing options. By understanding the genetic risks associated with GM2 disease, individuals can make informed decisions about family planning and genetic testing.
Individuals who are carriers of the HEXA or HEXB gene mutations associated with GM2 gangliosidosis have a 25% chance of passing on the faulty gene to each of their children٫ resulting in an affected offspring. Genetic counseling helps individuals assess their risk of carrying the genetic mutation and understand the implications for future generations.
Families affected by GM2 gangliosidosis may benefit from prenatal testing, which can identify the presence of genetic mutations in the developing fetus. This information enables families to make informed decisions about pregnancy management, including options for early intervention and family planning.
Preimplantation genetic diagnosis (PGD) offers individuals at risk of transmitting GM2 disease the opportunity to undergo in vitro fertilization (IVF) with genetic screening of embryos to select those free of the disease-causing mutations. This preventive approach can help reduce the likelihood of passing on GM2 gangliosidosis to future generations.
Genetic counselors work collaboratively with healthcare providers to offer personalized risk assessments, genetic testing options, and emotional support to individuals and families affected by GM2 gangliosidosis. By empowering individuals with knowledge about their genetic status, genetic counseling facilitates informed decision-making and promotes proactive healthcare management.
Education and awareness about the genetic implications of GM2 gangliosidosis are integral to promoting family health and well-being. By providing resources, guidance, and support, genetic counseling fosters a supportive environment for families navigating the complex challenges associated with these rare and devastating neurodegenerative disorders.
In conclusion, GM2 gangliosidosis, encompassing Tay-Sachs and Sandhoff diseases, represents a group of devastating neurodegenerative disorders characterized by the deficiency of the hexosaminidase A enzyme and the accumulation of GM2 gangliosides in cells. These progressive conditions present early in life with a range of neurological symptoms that worsen over time, leading to profound cognitive and motor impairment.
Diagnosis of GM2 disease involves a combination of clinical evaluation, enzymatic assays, and genetic testing to confirm the presence of Tay-Sachs or Sandhoff disease. While there is currently no curative treatment available, supportive care, symptom management, and palliative interventions play a critical role in addressing the complex needs of individuals affected by these relentless disorders.
Genetic counseling and family planning are essential components of comprehensive care for individuals at risk of GM2 gangliosidosis٫ offering insights into inheritance patterns٫ genetic testing options٫ and reproductive decision-making. By empowering individuals with knowledge about their genetic risks٫ genetic counseling enables informed choices and proactive healthcare management.
Ongoing research and innovative therapeutic strategies, such as enzyme replacement therapy and gene therapy, hold promise for advancing the management of GM2 gangliosidosis and improving outcomes for affected individuals in the future. By fostering collaboration between healthcare providers, researchers, and families, advancements in the field of lysosomal storage disorders offer hope for enhanced treatments and interventions.
Ultimately, raising awareness about GM2 gangliosidosis, promoting early detection, and providing comprehensive support for affected individuals and families are crucial steps in combating these challenging neurodegenerative diseases. Through continued research, education, and advocacy efforts, the medical community can work towards improving the quality of life and outcomes for those impacted by GM2 gangliosidosis.