Disease ⎻ Dihydropyrimidine Dehydrogenase Deficiency
Dihydropyrimidine dehydrogenase deficiency is a rare genetic disorder caused by mutations in the DPYD gene, leading to enzyme deficiency in pyrimidine metabolism. This can result in severe toxicity when individuals are treated with chemotherapy drugs like Fluorouracil. Pharmacogenomics and genetic testing play a crucial role in identifying patients at risk.
Introduction to Dihydropyrimidine Dehydrogenase Deficiency
Dihydropyrimidine dehydrogenase deficiency, a disorder related to pyrimidine metabolism, is caused by genetic variations in the DPYD gene. Individuals with this condition have reduced activity of the enzyme dihydropyrimidine dehydrogenase, crucial for metabolizing pyrimidines. When these individuals undergo chemotherapy with drugs like Fluorouracil, toxicity can occur due to the impaired metabolism of the drug. Understanding the genetic basis of this deficiency through pharmacogenomics and genetic testing is essential in predicting and preventing adverse reactions to chemotherapy. This introduction sets the stage for exploring the impact of this rare genetic disorder on patient care and the importance of personalized medicine in managing DPD deficiency.
Understanding Pyrimidine Metabolism
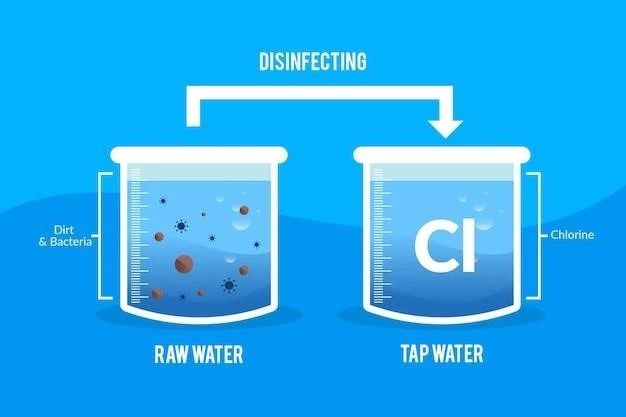
Pyrimidine metabolism is a crucial biochemical pathway in the body responsible for the synthesis and degradation of pyrimidine nucleotides, essential components of RNA and DNA. Dihydropyrimidine dehydrogenase (DPD) is a key enzyme in this pathway, playing a central role in the catabolism of uracil and thymine, which are pyrimidine bases. Genetic mutations in the DPYD gene can lead to a deficiency in the DPD enzyme, disrupting normal pyrimidine metabolism and causing toxicity when chemotherapy drugs like Fluorouracil are administered. Understanding the intricacies of pyrimidine metabolism is fundamental in comprehending the pathophysiology of Dihydropyrimidine dehydrogenase deficiency and its clinical implications. Through in-depth knowledge of this metabolic pathway, healthcare professionals can better manage patients with DPD deficiency and optimize treatment strategies to minimize adverse reactions.
Chemotherapy and Fluorouracil
Chemotherapy, a common cancer treatment, often includes Fluorouracil (5-FU), a medication used to treat various types of cancer, including colorectal, breast, and gastrointestinal cancers. Fluorouracil works by disrupting cancer cell growth through interfering with DNA and RNA synthesis. However, individuals with Dihydropyrimidine dehydrogenase deficiency face a higher risk of severe toxicity when treated with Fluorouracil due to their impaired ability to metabolize the drug. This heightened toxicity can lead to severe adverse effects, making personalized treatment strategies essential for patients with DPD deficiency. By understanding the impact of Fluorouracil on individuals with Dihydropyrimidine dehydrogenase deficiency, healthcare providers can tailor chemotherapy regimens to mitigate risks and optimize therapeutic outcomes.
Symptoms and Diagnosis
Individuals with Dihydropyrimidine dehydrogenase deficiency may experience a range of symptoms, including severe toxic reactions when exposed to chemotherapy drugs like Fluorouracil. These toxicities can manifest as gastrointestinal issues, myelosuppression, neurotoxicity, and dermatological effects. However, diagnosis of DPD deficiency is complex and often requires genetic testing to identify mutations in the DPYD gene. Additionally, measuring DPD enzyme activity levels in the blood or assessing urinary concentrations of metabolites can aid in confirming the deficiency. Prompt and accurate diagnosis of Dihydropyrimidine dehydrogenase deficiency is crucial in guiding treatment decisions and preventing potentially life-threatening complications associated with chemotherapy in affected individuals.
Pharmacogenomics and Genetic Testing
Pharmacogenomics, the study of how genes influence an individual’s response to medications, plays a pivotal role in managing Dihydropyrimidine dehydrogenase deficiency. Genetic testing is essential in identifying patients with mutations in the DPYD gene, predisposing them to enzyme deficiency in pyrimidine metabolism. By understanding a patient’s genetic makeup, healthcare providers can personalize treatment regimens, adjusting drug dosages or selecting alternative therapies to minimize the risk of adverse reactions to chemotherapy drugs like Fluorouracil. Genetic testing also enables early detection of DPD deficiency, allowing for proactive interventions and improved patient outcomes. The integration of pharmacogenomics and genetic testing into clinical practice can significantly enhance the safety and efficacy of chemotherapy treatments in individuals with Dihydropyrimidine dehydrogenase deficiency.
Treatment and Management
The treatment and management of Dihydropyrimidine dehydrogenase deficiency primarily focus on minimizing the risk of toxicity when administering chemotherapy, particularly Fluorouracil. For individuals identified with DPD deficiency through genetic testing, personalized medicine approaches are crucial. Strategies may include dose adjustments, alternative chemotherapy agents, or even opting for non-chemotherapeutic treatments depending on the specific genetic variants present. Close monitoring of adverse reactions and early intervention are essential in the management of patients with Dihydropyrimidine dehydrogenase deficiency. Collaborative care involving oncologists, pharmacists, and genetic counselors is imperative to ensure safe and effective treatment outcomes while minimizing the potential risks associated with chemotherapy in individuals with DPD deficiency.
Impact on Patient Care
Dihydropyrimidine dehydrogenase deficiency has a significant impact on patient care, particularly in the oncology setting. Individuals with this genetic disorder require specialized attention and tailored treatment plans to mitigate the risks associated with chemotherapy-induced toxicity. The incorporation of pharmacogenomic data and genetic testing results into clinical practice has revolutionized patient care by enabling healthcare providers to proactively identify individuals at increased risk for adverse drug reactions. By considering a patient’s genetic profile, healthcare teams can optimize treatment strategies, reduce unnecessary side effects, and improve treatment outcomes for individuals with DPD deficiency. The personalized approach to care for patients with Dihydropyrimidine dehydrogenase deficiency underscores the importance of precision medicine in oncology and reinforces the value of genetic testing in enhancing patient safety and treatment efficacy.
Future Directions and Research
Future directions in Dihydropyrimidine dehydrogenase deficiency research are oriented towards advancing the understanding of genetic variants associated with this condition and exploring innovative treatment modalities. Ongoing studies aim to elucidate the complex interactions between genetic factors, drug metabolism, and chemotherapy outcomes in individuals with DPD deficiency. Additionally, research endeavors are focused on developing novel pharmacogenomic approaches to predict and manage adverse drug reactions more effectively. Collaborative efforts between researchers, clinicians, and pharmaceutical industries are crucial in driving forward the field of personalized medicine for patients with Dihydropyrimidine dehydrogenase deficiency. By leveraging cutting-edge technologies and translational research, the future holds promise for improved diagnostic tools, targeted therapies, and optimized treatment algorithms for individuals affected by DPD deficiency.
Case Studies and Personal Stories
Exploring case studies and personal stories of individuals with Dihydropyrimidine dehydrogenase deficiency offers valuable insights into the real-world impact of this genetic disorder. These narratives shed light on the challenges faced by patients, healthcare providers, and families dealing with DPD deficiency. By sharing experiences and highlighting the journey of those affected by this condition, we can enhance awareness, empathy, and understanding within the medical community and society as a whole. Case studies and personal stories serve as powerful tools for advocating for personalized medicine approaches, genetic testing, and improved patient care for individuals with Dihydropyrimidine dehydrogenase deficiency. These accounts provide a human perspective on the complexities of managing a rare genetic disorder and underscore the importance of individualized treatment strategies tailored to each patient’s unique genetic makeup.
Conclusion
In conclusion, Dihydropyrimidine dehydrogenase deficiency represents a critical challenge in the field of oncology and personalized medicine. This rare genetic disorder, stemming from mutations in the DPYD gene, affects the metabolism of pyrimidines and poses significant risks for individuals undergoing chemotherapy, especially with drugs like Fluorouracil. The integration of pharmacogenomics and genetic testing has revolutionized the approach to managing DPD deficiency by enabling tailored treatment regimens based on individual genetic profiles. As research progresses and technology advances, there is hope for further advancements in diagnostics, treatment strategies, and patient care for those with Dihydropyrimidine dehydrogenase deficiency. By emphasizing precision medicine, genetic testing, and interdisciplinary collaboration, healthcare providers can optimize outcomes, enhance patient safety, and pave the way for a more personalized and effective approach to managing this complex genetic condition.