Disease ‒ LyP (Lymphomatoid Papulosis)
Introduction to LyP
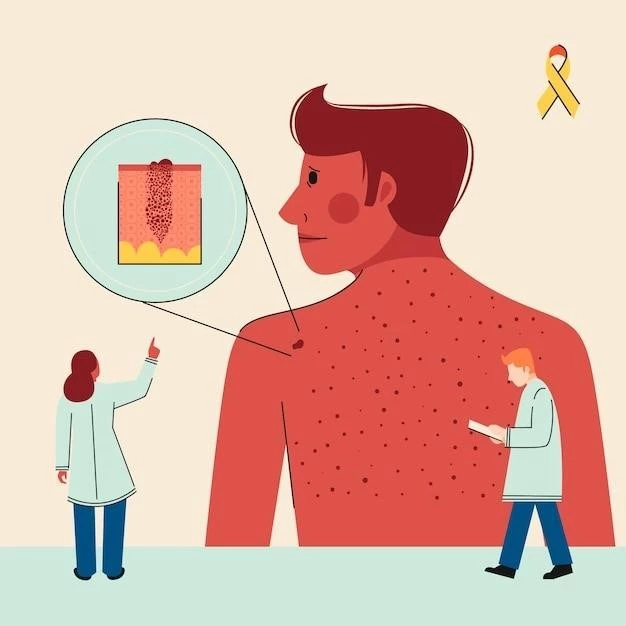
Lymphomatoid Papulosis (LyP) is a rare skin condition characterized by self-healing lymphoid papules or lesions. LyP belongs to the spectrum of primary cutaneous CD30-positive lymphoproliferative disorders. It is usually considered a chronic, indolent disorder that falls within the realm of cutaneous T-cell lymphomas.
Individuals with LyP often present with small, red or purple papules on the skin that may ulcerate or crust over before spontaneously regressing, leaving behind hyperpigmented spots. Despite sharing histological features with lymphoma, LyP is benign in nature and does not typically involve the internal organs.
The exact cause of LyP remains unclear, and it predominantly affects adults between the ages of 30 and 60. Given its self-limiting nature, LyP is thought to arise from an immune dysregulation, where T-cells in the skin react abnormally, triggering the characteristic skin lesions.
Diagnosing LyP usually involves a skin biopsy to examine the cellular composition of the lesions and rule out other forms of skin cancer. Distinguishing LyP from more aggressive forms of T-cell lymphoma is crucial for determining the appropriate management approach and prognosis.
Overall, understanding the distinct features of LyP is essential in ensuring accurate diagnosis and initiating timely treatment strategies to manage the condition effectively.
Understanding LyP
Lymphomatoid Papulosis (LyP) is a rare cutaneous condition classified as a form of blood cancer, specifically a lymphoid disorder that affects the skin. Despite sharing characteristics with malignant lymphomas, LyP is considered benign with a good prognosis in most cases.
LyP is characterized by the presence of self-healing papules or lesions on the skin that may come and go spontaneously over time. These lesions typically appear as small, red bumps that can evolve into ulcers before resolving, often leaving behind areas of hyperpigmentation.
Under a microscope, the lesions of LyP exhibit atypical lymphoid cells with CD30 expression, which distinguishes it from other skin disorders. The exact cause of LyP is unknown, but it is thought to involve abnormal immune system function, particularly a reactive response of T-cells in the skin.
Although LyP is primarily a skin disorder, in rare instances, it can progress to more aggressive forms of lymphoma. Therefore, accurate diagnosis through skin biopsies and monitoring by healthcare professionals are crucial to differentiate LyP from other lymphoid malignancies and determine the appropriate treatment approach.
Overall, having a comprehensive understanding of LyP is essential for healthcare providers to effectively diagnose, treat, and manage this uncommon condition, ensuring the best outcomes for individuals affected by this lymphoid papulosis.
Symptoms and Diagnosis
Individuals with Lymphomatoid Papulosis (LyP) often present with characteristic skin symptoms that include the appearance of small, red, or purple papules. These papules can evolve into ulcers, crust over, and eventually heal, leaving behind darkened spots on the skin; It is common for these lesions to come and go intermittently.
Diagnosing LyP typically involves a thorough examination of the skin lesions and a skin biopsy to analyze the cellular composition of the affected areas. The biopsy helps differentiate LyP from other skin conditions and aids in confirming the presence of atypical lymphoid cells expressing CD30, a hallmark of the disease.
Healthcare providers may also consider conducting additional tests, such as immunohistochemistry and molecular studies, to further characterize the lymphoid cells and rule out more aggressive forms of T-cell lymphoma. The diagnosis of LyP is essential for guiding appropriate treatment strategies and determining the prognosis of the condition.
Given the unique nature of LyP and its resemblance to malignant lymphomas, accurate diagnosis by experienced dermatologists or oncologists is paramount. Early detection and differentiation from other skin disorders are key to ensuring individuals receive the necessary care and interventions to manage this rare form of cutaneous lymphoid papulosis effectively.
Treatment Options for LyP
Managing Lymphomatoid Papulosis (LyP) typically involves a conservative approach due to its benign nature in most cases. Observation without intervention may be recommended for individuals with mild symptoms and limited skin involvement. Regular monitoring by healthcare providers is crucial to track any changes in the skin lesions.
In cases where symptomatic treatment is required, topical corticosteroids or phototherapy can be utilized to alleviate itching and inflammation associated with the lesions. These treatments aim to control symptoms and improve the overall appearance of the skin affected by LyP.
For individuals with more widespread or persistent lesions, systemic therapies such as methotrexate, retinoids, or low-dose chemotherapy agents may be considered. These agents target the abnormal lymphoid cells in the skin and can help induce remission or reduce the frequency of lesion recurrence.
In rare instances where LyP progresses to more aggressive forms of lymphoma, more intensive therapies such as radiation therapy or systemic biologic agents may be warranted. These treatments are typically reserved for cases where there is evidence of disease progression or involvement of internal organs.
Healthcare providers tailor treatment strategies for LyP based on the individual’s overall health status, the extent of skin involvement, and the presence of any associated symptoms. Close collaboration between dermatologists, oncologists, and other specialists is essential to ensure comprehensive care and optimal outcomes for individuals with this rare form of lymphoid papulosis.
Prognosis and Relapse
Individuals diagnosed with Lymphomatoid Papulosis (LyP) generally have a favorable prognosis, with the majority experiencing spontaneous remission of skin lesions over time. The condition is considered benign, and most cases do not progress to more aggressive forms of lymphoma.
Despite its generally indolent course, LyP can have periods of relapse, where new skin lesions may appear or existing ones may reoccur. Monitoring for relapse is crucial, and individuals should undergo regular follow-ups with healthcare providers to detect any changes in the skin or overall disease status.
In rare instances where LyP transforms into a more aggressive form of lymphoma, the prognosis may be less favorable, requiring more intensive treatments and close monitoring. Early detection of disease progression is essential in such cases to initiate appropriate therapies and optimize outcomes.
Overall, the prognosis for individuals with LyP is often excellent, especially when the disease remains confined to the skin and does not involve systemic organs. Continued surveillance and collaboration among healthcare teams are key in managing relapses, addressing any potential complications, and ensuring the best possible long-term outcomes for those affected by this rare cutaneous lymphoid disorder.
Achieving Remission
Attaining remission in Lymphomatoid Papulosis (LyP) is a primary goal of treatment, aiming to control and resolve the skin lesions associated with this rare condition. Remission can be achieved through various therapeutic interventions tailored to the individual’s specific disease presentation and response to treatment.
For many individuals with LyP, achieving remission involves the use of topical corticosteroids, phototherapy, or systemic agents such as methotrexate or retinoids to target the abnormal lymphoid cells in the skin. These treatments aim to reduce inflammation, halt lesion progression, and promote the healing of existing papules.
Monitoring the response to treatment is critical in assessing the effectiveness of therapy and guiding adjustments to optimize outcomes. Healthcare providers may recommend regular follow-up visits and imaging studies to evaluate the extent of disease involvement and monitor for any signs of relapse.
In some cases, achieving remission in LyP may require a multidisciplinary approach involving dermatologists, oncologists, and other specialists to ensure comprehensive care and management. Close collaboration among healthcare teams can help tailor treatment strategies, address any underlying immune dysregulation, and support individuals in achieving sustained remission.
Overall, the goal of achieving remission in LyP is essential in improving symptoms, preventing disease progression, and enhancing the quality of life for individuals affected by this lymphoid papulosis. With appropriate treatment and ongoing monitoring, many individuals with LyP can successfully enter and maintain remission, allowing them to lead fulfilling and healthy lives.
Coping with LyP
Coping with Lymphomatoid Papulosis (LyP) involves a holistic approach to managing the physical, emotional, and psychological aspects of living with this rare skin condition. Individuals diagnosed with LyP may experience various challenges related to the unpredictability of skin lesions, potential relapses, and the impact on overall well-being.
Seeking support from healthcare professionals, including dermatologists, oncologists, and counselors, can help individuals navigate the complexities of LyP and address any concerns or anxieties they may have. Open communication with healthcare providers is vital in understanding the condition, treatment options, and developing coping strategies.
Engaging in self-care practices such as maintaining a healthy lifestyle, managing stress effectively, and adhering to prescribed treatment regimens can positively impact the management of LyP. Establishing a routine for skin care, monitoring skin changes, and reporting any new symptoms promptly can empower individuals in taking an active role in their health.
Connecting with support groups, online communities, or local organizations specializing in skin conditions can provide a sense of community and solidarity for individuals living with LyP. Sharing experiences, tips, and resources with others facing similar challenges can offer valuable support and encouragement.
Embracing a positive outlook, staying informed about the latest advancements in the management of LyP, and maintaining a strong support network of family and friends can help individuals cope effectively with the uncertainties associated with this unique cutaneous lymphoid disorder.
Conclusion
In conclusion, Lymphomatoid Papulosis (LyP) represents a rare form of cutaneous lymphoid disorder characterized by self-healing papules or lesions on the skin. Despite sharing histological features with malignant lymphomas, LyP is generally considered benign with a favorable prognosis in most cases.
Understanding the distinct features of LyP, including its indolent nature, potential for relapse, and rare progression to more aggressive forms of lymphoma, is paramount in guiding accurate diagnosis and appropriate treatment interventions. Healthcare providers play a significant role in monitoring disease progression, implementing tailored treatment strategies, and supporting individuals in achieving remission.
By adopting a multidisciplinary approach that encompasses dermatological, oncological, and psychological support, individuals living with LyP can effectively manage the physical and emotional challenges associated with the condition. Accessing resources, engaging in self-care practices, and connecting with support networks can empower individuals to cope with the uncertainties of living with this unique skin disorder.
Ultimately, ongoing research efforts, advancements in treatment modalities, and improved patient awareness contribute to enhancing the management of LyP and optimizing outcomes for affected individuals. By promoting education, fostering resilience, and encouraging collaboration among healthcare professionals and individuals with LyP, we aim to improve the quality of life and well-being of those living with this rare cutaneous lymphoid papulosis.