Article Plan⁚ Disease — Myxomatous Peritonitis
Overview of Myxomatous Peritonitis
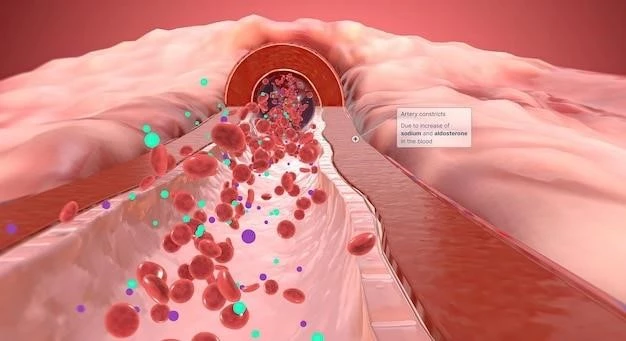
Pseudomyxoma peritonei (PMP) is a rare clinical entity characterized by diffuse intra-abdominal gelatinous ascites with mucinous implants on peritoneal surfaces. It is caused by cancerous cells (mucinous adenocarcinoma) producing abundant mucin, leading to fibrosis of tissues and impairment of organ functions. This slow-growing type of abdominal cancer primarily affects the peritoneum. Myxomatous peritonitis, a condition associated with gelatinous mucin filling the peritoneal cavity, is a significant aspect of PMP. The condition can result in severe complications, including bowel obstruction and organ compression, potentially leading to life-threatening outcomes if left untreated.
Causes and Risk Factors
Myxomatous peritonitis, which is a significant aspect of pseudomyxoma peritonei, is primarily caused by cancerous cells known as mucinous adenocarcinoma that produce excessive mucin or gelatinous ascites. This condition arises from mucinous neoplasms, with low-grade or high-grade appendiceal mucinous neoplasms being the primary culprits. While appendiceal primary cancer is the most common cause, mucinous tumors of the ovary can also be implicated. Factors such as genetic predisposition or environmental influences may contribute to the development of this rare and indolent form of abdominal cancer.
Symptoms and Diagnosis
Identification of myxomatous peritonitis, a key component of pseudomyxoma peritonei, often involves symptoms like abdominal distension, discomfort, and pain. As the gelatinous mucin accumulates, it can lead to organ compression, causing issues with bowel movements and digestion. Diagnosing this condition typically involves imaging tests such as CT scans or MRIs to visualize the extent of mucin spread within the peritoneal cavity. Biopsies may be performed to confirm the presence of mucinous adenocarcinoma cells, aiding in a definitive diagnosis.
Treatment Options
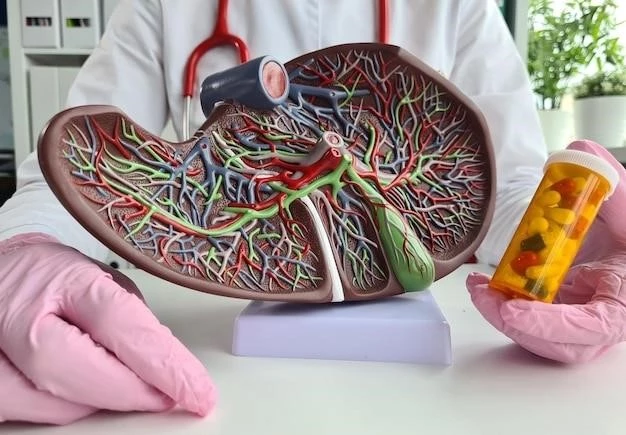
The treatment of myxomatous peritonitis often involves a combination of strategies tailored to each individual’s case. Surgery, particularly cytoreductive surgery, plays a central role in removing visible tumor masses and mucin from the abdominal cavity. Hyperthermic intraperitoneal chemotherapy (HIPEC) may be utilized during surgery to target any remaining cancer cells. Postoperative intraperitoneal chemotherapy or systemic chemotherapy may be recommended to prevent recurrence. Close monitoring and follow-up care are crucial to assess response to treatment and address any complications that may arise.
Complications and Prognosis
Complications of myxomatous peritonitis, a component of pseudomyxoma peritonei, can include bowel obstruction, organ compression, and malnourishment due to impaired digestion. The prognosis for individuals with this condition varies depending on factors such as the extent of tumor spread and response to treatment. Close monitoring for potential complications such as acute appendicitis and intra-abdominal sepsis is essential to manage this rare and indolent form of abdominal cancer effectively.
Prevention Strategies
Preventing myxomatous peritonitis, a key aspect of pseudomyxoma peritonei, primarily involves early detection and comprehensive treatment of mucinous neoplasms in organs such as the appendix and ovaries. Regular medical check-ups and screening for any suspicious abdominal symptoms can aid in the early diagnosis of potential cancerous growths. Adhering to a healthy lifestyle, including a balanced diet and regular exercise, may help reduce the risk of developing conditions that could lead to myxomatous peritonitis.
Research and Future Directions
Ongoing research in the field of myxomatous peritonitis primarily focuses on improving diagnostic techniques to identify the condition at earlier stages, potentially leading to better treatment outcomes. Future directions include exploring targeted therapies that aim to inhibit mucin production in cancerous cells, thereby reducing the accumulation of gelatinous ascites in the peritoneal cavity. Investigating the genetic and molecular mechanisms underlying this rare disease may pave the way for personalized treatment approaches that target specific pathways related to myxomatous peritonitis.