Disease ⏤ Irritable Bowel Syndrome
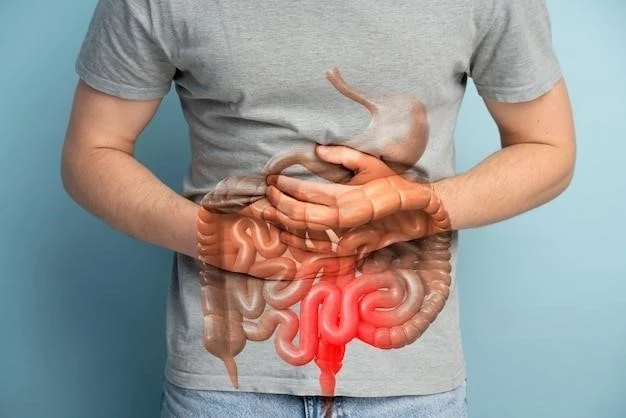
Irritable Bowel Syndrome, commonly known as IBS, is a chronic gastrointestinal disorder that affects the large intestine. It is characterized by symptoms such as abdominal pain, diarrhea, constipation, bloating, gas, cramping, and discomfort. The exact cause of IBS is unknown, but factors like inflammation, abnormal bowel movements, stress, diet, and certain trigger factors play a role in its development.
I. Introduction to Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a common disorder that affects the large intestine, leading to a variety of symptoms that can significantly impact a person’s quality of life. The exact cause of IBS remains unclear, making it a complex condition to diagnose and treat.
Individuals with IBS experience a range of gastrointestinal symptoms such as abdominal pain, bloating, gas, cramping, and changes in bowel habits, including diarrhea and constipation. These symptoms can vary in severity and duration, often recurring over an extended period.
IBS is considered a functional gastrointestinal disorder, meaning there is no structural or biochemical explanation for the symptoms. It is diagnosed based on a combination of symptoms, medical history, physical examination, and sometimes additional tests to rule out other conditions.
The impact of IBS extends beyond the physical symptoms, as it can also affect a person’s emotional well-being and overall quality of life. Coping with the unpredictable nature of the condition and managing symptoms on a daily basis can be challenging and stressful for individuals with IBS.
Understanding the underlying mechanisms of IBS, as well as the factors that contribute to its development, is essential for effective management and treatment. By exploring the causes and triggers of IBS, healthcare professionals can work towards providing personalized care and support to individuals living with this chronic disorder.
II. Symptoms of Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) manifests through a variety of symptoms that can vary in intensity and frequency among individuals. The most common symptoms of IBS include⁚
- Abdominal Pain⁚ Individuals with IBS often experience recurrent abdominal pain or discomfort that is typically relieved or worsened after a bowel movement.
- Diarrhea⁚ Some people with IBS experience diarrhea, characterized by loose or watery stools, which can be accompanied by urgency and a feeling of incomplete emptying.
- Constipation⁚ Others may have constipation, where bowel movements are infrequent or difficult, often accompanied by straining and a sensation of incomplete evacuation.
- Bloating⁚ Bloating is a common symptom of IBS, leading to a sensation of fullness, tightness, or discomfort in the abdomen.
- Gas⁚ Excessive gas or flatulence is another symptom that individuals with IBS may experience, contributing to bloating and abdominal distension.
- Cramping⁚ Abdominal cramping and spasms are prevalent in IBS and can range from mild to severe, causing significant discomfort.
- Discomfort⁚ Overall discomfort in the abdominal region is a hallmark of IBS and can impact daily activities and quality of life.
It is essential to recognize the diverse nature of symptoms associated with IBS as they can fluctuate over time and be influenced by various factors such as stress, diet, hormonal changes, and medication use. Monitoring symptoms and seeking appropriate medical advice can help individuals manage their condition effectively and improve their overall well-being.
III. Causes and Triggers of Irritable Bowel Syndrome
The exact causes of Irritable Bowel Syndrome (IBS) are not fully understood, and it is believed to result from a complex interplay of various factors. While the precise etiology remains elusive, several theories suggest potential contributors to the development of this gastrointestinal disorder.
One proposed factor is altered gastrointestinal motility, where the normal contractions of the intestines may be irregular or uncoordinated in individuals with IBS. This dysregulation can lead to symptoms such as diarrhea, constipation, and abdominal discomfort.
Abnormalities in the gut-brain axis have also been implicated in IBS, highlighting the communication between the brain and the gut. Changes in the central nervous system’s processing of pain signals and alterations in neurotransmitters, such as serotonin, may influence gut function and sensitivity in individuals with IBS.
Inflammation within the intestines is another potential trigger for IBS symptoms, even though it does not present with the same structural damage seen in inflammatory bowel diseases like Crohn’s disease or ulcerative colitis. Low-grade inflammation and immune system dysregulation could contribute to the pathophysiology of IBS.
Psychological factors, such as stress, anxiety, and depression, can play a significant role in exacerbating IBS symptoms. The gut-brain connection is bidirectional, meaning that emotional distress can impact gut function, leading to symptoms like abdominal pain, bloating, and altered bowel habits.
Dietary factors are commonly reported triggers for IBS symptoms, with certain foods and beverages exacerbating gastrointestinal discomfort and irregularities. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten, dairy, and caffeine are examples of dietary components that may provoke symptoms in susceptible individuals.
Furthermore, lifestyle factors, medication use, hormonal fluctuations, and even environmental influences can act as triggers for IBS symptoms. By identifying and understanding these causative and precipitating factors, healthcare providers can tailor management strategies to address the specific needs of individuals with IBS and enhance their overall quality of life.
IV. Diagnosing Irritable Bowel Syndrome
Diagnosing Irritable Bowel Syndrome (IBS) involves a comprehensive evaluation of a patient’s symptoms, medical history, physical examination, and selective testing to rule out other potential gastrointestinal conditions. Due to the absence of specific diagnostic markers or definitive tests for IBS, healthcare providers rely on established criteria and clinical judgment to make an accurate diagnosis.
The Rome criteria, particularly the Rome IV criteria, are widely used in the diagnosis of IBS. These criteria focus on the presence of characteristic gastrointestinal symptoms, including abdominal pain or discomfort for a specified duration, as well as the frequency and nature of bowel movements. Meeting these criteria aids in distinguishing IBS from other gastrointestinal disorders.
Medical history plays a crucial role in the diagnostic process, as it helps healthcare providers understand the onset, duration, and progression of symptoms experienced by the individual. Patients may be asked to provide details about their bowel habits, diet, stressors, medications, and other relevant factors that could contribute to their gastrointestinal complaints.
Physical examination is conducted to assess abdominal tenderness, bloating, and any signs of abnormalities that may suggest an alternate diagnosis. While physical findings may be relatively nonspecific in IBS, they can guide healthcare providers in evaluating the patient’s overall health and identifying potential red flags that warrant further investigation.
Diagnostic testing may be recommended to rule out other conditions that mimic IBS symptoms, such as inflammatory bowel diseases, celiac disease, or colorectal cancer. Tests may include blood work to check for signs of inflammation or anemia, stool studies to assess for infections or malabsorption, and imaging studies like colonoscopy or flexible sigmoidoscopy to visualize the intestinal lining.
Additionally, hydrogen breath tests may be performed to evaluate for conditions like small intestinal bacterial overgrowth (SIBO) or lactose intolerance, which can present with symptoms similar to those of IBS. These tests help exclude other potential causes of gastrointestinal distress and assist in confirming an IBS diagnosis.
Overall, the diagnostic process for IBS involves a comprehensive approach that considers the patient’s symptoms, medical history, physical examination findings, and selective testing to establish a precise diagnosis. Collaboration between healthcare providers and patients is essential in navigating the complexities of IBS diagnosis and ensuring appropriate management strategies are implemented for optimal care.
V. Treatment Options for Irritable Bowel Syndrome
Managing Irritable Bowel Syndrome (IBS) involves a multifaceted approach aimed at alleviating symptoms, improving quality of life, and addressing the underlying factors contributing to the condition. Treatment strategies for IBS incorporate lifestyle modifications, dietary changes, behavioral therapies, and, in some cases, medications to achieve symptom control and long-term management.
Diet Modification⁚ Adjusting dietary habits is a cornerstone of IBS management. Following a low-FODMAP diet, which restricts fermentable carbohydrates known to trigger symptoms, or identifying and avoiding specific trigger foods can help reduce gastrointestinal distress. Additionally, adequate fiber intake, hydration, and regular meals can promote digestive health.
Stress Management⁚ Stress is a common exacerbating factor for IBS symptoms. Stress reduction techniques such as mindfulness, relaxation exercises, yoga, and cognitive-behavioral therapy can help individuals manage stress and improve their overall well-being. Establishing a healthy work-life balance and prioritizing self-care are also beneficial.
Medications⁚ Pharmacological agents may be prescribed to target specific symptoms of IBS. Antispasmodics can help alleviate abdominal cramping, while laxatives or antidiarrheals may be used to regulate bowel movements. Probiotics, antibiotics for bacterial overgrowth, and antidepressants for pain modulation and mood enhancement are among the pharmaceutical options available.
Behavioral Therapies⁚ Cognitive-behavioral therapy (CBT) and gut-directed hypnotherapy have shown efficacy in managing IBS symptoms by addressing psychological factors and modifying maladaptive behaviors. These therapeutic approaches aim to enhance coping skills, reduce symptom perception, and improve overall quality of life for individuals with IBS.
Exercise and Physical Activity⁚ Regular physical activity can benefit individuals with IBS by promoting bowel regularity, reducing stress, and enhancing overall health. Engaging in low-impact exercises like walking, yoga, or swimming can aid in symptom management and contribute to a sense of well-being.
Symptom Monitoring⁚ Keeping a symptom diary to track triggers, symptom patterns, and treatment effectiveness can help individuals and healthcare providers identify personalized strategies for symptom control. Open communication with healthcare professionals is essential to adjusting treatment plans and ensuring optimal care.
By combining various treatment modalities tailored to the individual’s needs, individuals with IBS can effectively manage their symptoms, reduce the frequency and severity of flare-ups, and improve their overall quality of life. Empowering patients with knowledge, self-care strategies, and ongoing support is key to achieving successful outcomes in the management of Irritable Bowel Syndrome.
VI. Medications for Irritable Bowel Syndrome
Medications play a crucial role in the management of Irritable Bowel Syndrome (IBS) by targeting specific symptoms and underlying mechanisms that contribute to gastrointestinal discomfort. Different classes of medications are available to help individuals alleviate symptoms, improve bowel function, and enhance quality of life.
Antispasmodics⁚ Antispasmodic medications such as hyoscyamine, dicyclomine, and peppermint oil can help reduce abdominal cramping and spasms in individuals with IBS. These medications work by relaxing smooth muscle in the intestines, easing pain and discomfort associated with gut contractions.
Antidiarrheal Agents⁚ For individuals experiencing diarrhea-predominant IBS, medications like loperamide (Imodium) can help slow down bowel movements and improve stool consistency. By reducing the frequency and urgency of diarrhea, antidiarrheal agents can provide relief and enhance bowel control.
Laxatives⁚ Constipation is a common symptom in a subset of individuals with IBS. Osmotic laxatives, stool softeners, and fiber supplements can help promote regular bowel movements and alleviate constipation-related discomfort; It is essential to use laxatives under medical supervision to prevent dependency.
Probiotics⁚ Probiotic supplements containing beneficial bacteria strains may offer gastrointestinal benefits for individuals with IBS. Probiotics can help restore gut microbiota balance, improve digestion, reduce inflammation, and enhance immune function. Research supports the potential of probiotics in alleviating IBS symptoms.
Tricyclic Antidepressants⁚ Tricyclic antidepressants like amitriptyline and nortriptyline are sometimes prescribed for individuals with IBS to modulate pain perception and improve mood. These medications can have analgesic effects in lower doses than those required for treating depression, making them valuable in managing IBS-related discomfort.
Serotonin Modulators⁚ Medications that target serotonin receptors in the gut, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), may be beneficial for individuals with IBS. These medications can help regulate intestinal motility, visceral sensitivity, and mood, contributing to symptom control.
Antibiotics⁚ In cases of suspected small intestinal bacterial overgrowth (SIBO) or bacterial imbalances in the gut microbiota, antibiotics may be prescribed to reduce bacterial overgrowth and alleviate symptoms of bloating, gas, and altered bowel habits. Antibiotic therapy is targeted and may require additional probiotic supplementation.
It is essential for healthcare providers to individualize medication regimens for each patient based on their predominant symptoms, medical history, comorbidities, and treatment response. Regular monitoring, dosage adjustments, and potential side effect management are key considerations in optimizing medication therapy for Irritable Bowel Syndrome.
VII. Lifestyle Changes and Coping Strategies
Integrating lifestyle modifications and coping strategies into daily routines is paramount for effectively managing Irritable Bowel Syndrome (IBS) and improving overall well-being. By adopting healthy habits and implementing stress-reducing techniques, individuals can mitigate symptoms, enhance quality of life, and promote gastrointestinal health.
Dietary Modifications⁚ Following a well-balanced diet that includes adequate fiber, hydration, and individualized food triggers plays a significant role in managing IBS symptoms. Keeping a food diary to identify trigger foods, practicing mindful eating, and working with a healthcare provider or dietitian to create a tailored eating plan can help optimize digestive comfort.
Regular Physical Activity⁚ Engaging in regular exercise not only promotes physical fitness but also supports digestive function and stress management. Low-impact activities such as walking, yoga, swimming, or cycling can aid in bowel regularity, reduce bloating, and alleviate tension in the body, contributing to symptom relief.
Stress Management Techniques⁚ Stress can exacerbate IBS symptoms; therefore, learning and practicing stress-reducing techniques are essential. Mindfulness meditation, deep breathing exercises, progressive muscle relaxation, and yoga can help individuals cope with stress, promote relaxation, and modulate the body’s response to emotional triggers.
Adequate Sleep⁚ Prioritizing restful sleep is crucial for overall health and well-being, including managing IBS symptoms. Establishing a consistent sleep routine, creating a conducive sleep environment, and practicing good sleep hygiene habits can improve gastrointestinal function, support immune health, and enhance resilience to stress.
Hydration⁚ Maintaining proper hydration levels is vital for digestive health and symptom management in individuals with IBS. Drinking an adequate amount of water throughout the day can help prevent constipation, support bowel regularity, and reduce the risk of dehydration, which can exacerbate gastrointestinal discomfort.
Support Networks⁚ Building a strong support network of family, friends, healthcare providers, or support groups can offer emotional encouragement, practical advice, and a sense of community for individuals living with IBS. Sharing experiences, seeking advice, and receiving empathy from others can positively impact coping strategies and overall psychological well-being.
Time Management⁚ Effective time management skills can help individuals reduce stress, minimize triggers, and maintain a sense of control over their daily routines. Prioritizing tasks, setting realistic goals, delegating responsibilities, and allowing time for self-care activities are essential for balancing commitments and managing IBS-related challenges.
By incorporating lifestyle changes, stress-reducing techniques, and coping strategies into daily life, individuals with Irritable Bowel Syndrome can proactively manage their condition, alleviate symptoms, and enhance overall quality of life. Tailoring these approaches to individual preferences and needs can empower individuals to take control of their health and well-being in the face of this chronic gastrointestinal condition.
VIII. Prevention and Long-Term Management of Irritable Bowel Syndrome
Effective prevention and long-term management strategies are essential for individuals living with Irritable Bowel Syndrome (IBS) to minimize symptoms, improve quality of life, and promote gastrointestinal health in the long run. By taking a proactive approach towards symptom control and overall well-being, individuals can better navigate the challenges associated with this chronic condition.
Identify Trigger Factors⁚ Understanding individual trigger factors that exacerbate IBS symptoms is crucial for prevention and management. Keeping a symptom diary, tracking food intake, stress levels, and environmental influences can help identify triggers and allow for targeted intervention strategies.
Maintain a Healthy Diet⁚ Following a balanced diet that includes fiber-rich foods, adequate hydration, and limited intake of known trigger foods is key to managing IBS symptoms. Avoiding high FODMAP foods, spicy dishes, caffeine, and alcohol can reduce gastrointestinal distress and support digestive comfort.
Regular Physical Activity⁚ Incorporating regular exercise into daily routines can aid in bowel regularity, stress reduction, and overall well-being for individuals with IBS. Engaging in low-impact activities such as walking, yoga, or swimming can promote gastrointestinal motility and enhance symptom management.
Stress Management Techniques⁚ Implementing stress management techniques such as deep breathing, meditation, progressive muscle relaxation, and mindfulness can help reduce the impact of stress on IBS symptoms. Developing coping mechanisms to handle stressful situations effectively is essential for long-term symptom control.
Medication Adherence⁚ Following prescribed medication regimens as directed by healthcare providers is vital for symptom management and long-term control of IBS. Communicating any medication-related concerns or side effects to healthcare professionals and attending regular follow-up appointments can optimize treatment outcomes.
Monitor Symptoms and Progress⁚ Regularly monitoring symptoms, tracking treatment efficacy, and noting changes in bowel habits can help individuals gauge their progress and make informed decisions regarding their care. Open communication with healthcare providers and timely adjustments to treatment plans are critical for long-term management.
Seek Professional Support⁚ Consulting healthcare providers, gastroenterologists, dietitians, or mental health professionals for personalized guidance and support is essential for effective long-term management of IBS. Collaborating with a multidisciplinary team can ensure comprehensive care and address individual needs for optimal symptom control.
Lifestyle Maintenance⁚ Maintaining healthy lifestyle habits, such as adequate sleep, hydration, regular exercise, and balanced nutrition, is fundamental for managing IBS symptoms over the long term. Establishing consistent routines, setting realistic goals, and prioritizing self-care activities can contribute to sustained symptom relief.
By adopting preventive measures, adhering to treatment plans, and implementing long-term management strategies tailored to individual needs, individuals with Irritable Bowel Syndrome can effectively control symptoms, enhance quality of life, and foster gastrointestinal health for the future. Empowering individuals to take an active role in their care and well-being is key to achieving sustained relief and long-term success in managing this chronic gastrointestinal condition.
