Disease — Great Vessels Transposition
Introduction to Great Vessels Transposition
Great Vessels Transposition, a complex congenital heart defect, involves abnormal positioning of the main arteries — the aorta and pulmonary artery ⎻ leading to disrupted blood circulation and oxygenation. This condition requires timely diagnosis and surgical intervention to redirect blood flow, ensuring proper oxygen supply to the body. Understanding the causes, risk factors, symptoms, diagnostic methods, treatment options, and potential complications associated with Great Vessels Transposition is crucial for the effective management and care of affected infants. Collaboration between pediatricians, cardiologists, and specialized healthcare providers is essential to improve survival rates and long-term outcomes.
Understanding the Condition
Great Vessels Transposition is a critical congenital heart defect where the main arteries are improperly connected, leading to disrupted blood flow and oxygenation. Babies born with this condition require immediate medical attention to correct the abnormal positioning of arteries and ensure adequate oxygen supply to the body. Understanding the complexities of Great Vessels Transposition, including its various types and potential impact on the cardiovascular system, is essential for accurate diagnosis and effective treatment planning. Cooperation between pediatricians, cardiologists, and genetic specialists is key to providing optimal care and managing the condition’s challenges.
Definition and Overview of Great Vessels Transposition
Great Vessels Transposition is a congenital heart defect characterized by the abnormal positioning of the aorta and pulmonary artery, resulting in improper blood circulation and oxygenation. This condition hinders the body’s ability to receive oxygenated blood efficiently, leading to serious health complications. Understanding the specifics of Great Vessels Transposition, including how the defect affects blood flow and heart function, is crucial for diagnosing and managing the condition effectively. Collaboration between healthcare professionals, including cardiologists and pediatricians, is essential to provide comprehensive care and improve outcomes for infants with this complex cardiac anomaly.
Types of Congenital Heart Defects in Great Vessels Transposition
Within the spectrum of Great Vessels Transposition, several variations of congenital heart defects may occur, including double outlet right ventricle and ventricular septal defect. These defects contribute to the abnormal blood flow patterns and oxygenation issues observed in patients with Great Vessels Transposition. Recognizing the specific types of heart anomalies present in each case is vital for tailoring treatment strategies to address the unique cardiovascular challenges faced by affected infants. A thorough understanding of the variations in congenital heart defects associated with Great Vessels Transposition enables healthcare providers to deliver personalized and effective care to optimize outcomes and enhance the quality of life for these patients.
Causes and Risk Factors
The development of Great Vessels Transposition is often influenced by a combination of genetic factors and congenital abnormalities during fetal growth. Genetic predispositions and mutations can play a significant role in the occurrence of this complex heart defect. Additionally, certain environmental factors, such as maternal health conditions or exposures during pregnancy, may increase the risk of Great Vessels Transposition in newborns. Understanding the interplay between genetic predisposition and environmental influences is essential for assessing the risks associated with this congenital condition. Identifying and addressing these causes and risk factors early on is crucial for timely diagnosis, intervention, and improving the outcomes for infants with Great Vessels Transposition.
Genetic Factors and Congenital Abnormalities
Great Vessels Transposition is closely linked to genetic factors and congenital abnormalities that affect the development of the cardiovascular system during embryonic stages. Mutations in specific genes responsible for heart formation can lead to the misalignment of major arteries, resulting in this congenital heart defect. Various chromosomal anomalies and inherited conditions have been associated with an increased risk of Great Vessels Transposition. Understanding the genetic basis of this condition is crucial for genetic counseling, early detection, and personalized treatment planning. Genetic testing and evaluation are essential components in identifying underlying genetic factors contributing to the development of Great Vessels Transposition.
Environmental Risk Factors
Environmental risk factors can also contribute to the development of Great Vessels Transposition, particularly during prenatal stages. Maternal health conditions such as diabetes, alcohol consumption, or exposure to certain medications or toxins can increase the risk of congenital heart defects in the fetus, including Great Vessels Transposition. Adequate prenatal care, including screenings and monitoring, is essential to identify and mitigate potential environmental risk factors that may impact fetal heart development. By addressing environmental factors that can influence the occurrence of this complex heart defect, healthcare providers can work towards reducing the risk and improving the outcomes for infants affected by Great Vessels Transposition.

Diagnosis and Evaluation
Diagnosing Great Vessels Transposition typically involves a comprehensive evaluation of the infant’s symptoms, medical history, and physical examination by a pediatrician or cardiologist. Specialized diagnostic tests such as echocardiograms, MRI scans, and CT scans play a crucial role in confirming the presence of this congenital heart defect and assessing its severity. These imaging techniques provide detailed insights into the structural abnormalities of the heart and the positioning of major arteries, enabling healthcare providers to formulate an appropriate treatment plan. Early and accurate diagnosis through a combination of clinical assessment and advanced imaging modalities is essential for initiating timely interventions and optimizing outcomes for infants with Great Vessels Transposition.
Symptoms and Signs of Great Vessels Transposition in Infants
Infants with Great Vessels Transposition may exhibit symptoms such as rapid breathing, poor feeding, bluish skin discoloration (cyanosis), and fatigue. The characteristic signs of this congenital heart defect include a heart murmur and abnormalities in heart rhythm. These clinical manifestations indicate the disruption of oxygen-rich and oxygen-poor blood circulation, necessitating prompt medical evaluation. Recognizing these symptoms early is crucial for timely diagnosis and intervention to address the abnormal positioning of major arteries and optimize oxygen supply. Vigilant monitoring of infants for these specific signs is essential for identifying Great Vessels Transposition and initiating appropriate treatment measures.
Diagnostic Tests⁚ Echocardiogram, MRI, CT scans
Diagnostic evaluation of Great Vessels Transposition often involves advanced imaging techniques such as echocardiograms, MRI scans, and CT scans. An echocardiogram uses sound waves to create detailed images of the heart’s structure and function, allowing healthcare providers to assess the positioning of major arteries. MRI and CT scans provide further clarity on cardiac anatomy and blood flow patterns, aiding in the accurate diagnosis and severity assessment of this congenital heart defect. These diagnostic tests play a pivotal role in guiding treatment decisions and surgical interventions by providing crucial insights into the intricate cardiovascular abnormalities associated with Great Vessels Transposition.
Treatment Options
Treating Great Vessels Transposition often involves surgical interventions to correct the abnormal positioning of arteries and restore proper blood circulation. Arterial switch operation is a common procedure where the aorta and pulmonary artery are realigned to ensure efficient oxygenation. In some cases, medication therapy may be used to stabilize the infant’s condition before or after surgery. The goal of treatment is to improve oxygen delivery to the body and prevent complications associated with inadequate blood flow. Collaborative care involving pediatricians, cardiologists, and cardiac surgeons is essential to determine the most suitable treatment approach based on the individual needs of the infant with Great Vessels Transposition.
Surgical Interventions for Great Vessels Transposition
Surgical treatment for Great Vessels Transposition primarily involves procedures like arterial switch operation, where the aorta and pulmonary artery are surgically repositioned to restore normal blood flow patterns. This intervention aims to correct the congenital heart defect and optimize oxygen supply throughout the body. Other surgical techniques may include septal defect closure or coronary artery reimplantation to address associated abnormalities. The expertise of cardiac surgeons in performing these intricate procedures is vital for ensuring successful outcomes and improving the long-term prognosis of infants with Great Vessels Transposition. Close post-operative monitoring and follow-up care are essential components of the comprehensive management of this complex cardiac condition;
Medications and Therapies
In addition to surgical interventions, medications and therapies play a vital role in managing Great Vessels Transposition. Medications like prostaglandin E1 can help stabilize blood flow and improve oxygen levels before surgical correction. Post-surgery, medications may be prescribed to manage symptoms, prevent infections, and support heart function. Non-pharmacological therapies such as nutritional support and developmental interventions are also essential for the holistic care of infants with this congenital heart defect. Collaborative efforts between healthcare providers, including cardiologists, pediatricians, and allied healthcare professionals, are crucial for implementing a comprehensive treatment plan that addresses both the medical and developmental needs of infants with Great Vessels Transposition.
Complications Associated with Great Vessels Transposition
Great Vessels Transposition can lead to various complications affecting the cardiovascular system, such as abnormal blood flow, inadequate oxygenation, and impaired heart function. These complications may result in issues like heart failure, arrhythmias, and developmental delays due to reduced oxygen supply to vital organs. Moreover, surgical interventions to correct the defect may carry risks of bleeding, infection, or long-term cardiac issues. Close monitoring for complications post-treatment is crucial for early detection and prompt management. Healthcare providers must address these potential complications proactively to ensure optimal outcomes and quality of life for infants with Great Vessels Transposition.
Impact on Arteries and Veins
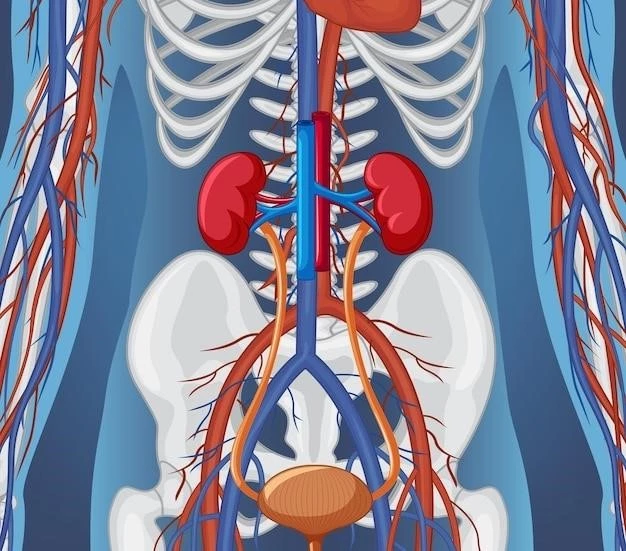
Great Vessels Transposition exerts a profound impact on the arteries and veins within the cardiovascular system. The improper positioning of the aorta and pulmonary artery disrupts the normal blood flow, leading to issues with oxygenation and circulation. This condition can strain the heart and blood vessels, potentially resulting in complications such as hypertension or vascular abnormalities. The altered blood flow patterns can also affect the lungs, brain, and other vital organs, impacting overall health and development. Addressing the impact on arteries and veins through surgical correction and post-operative care is critical in minimizing long-term vascular complications and optimizing cardiac function in individuals with Great Vessels Transposition.
Blood Circulation and Oxygenation Issues
Great Vessels Transposition significantly impacts blood circulation and oxygenation in the body. The abnormal positioning of major arteries disrupts the systemic and pulmonary circulation, leading to a mismatch in oxygen-rich and oxygen-poor blood distribution. This results in decreased oxygen levels reaching tissues and organs, affecting overall function and development. Addressing these circulation and oxygenation issues is vital to prevent complications like organ damage or heart failure. Timely surgical intervention and ongoing management aim to restore proper blood flow patterns and enhance oxygen delivery, ensuring better health outcomes and quality of life for individuals affected by Great Vessels Transposition.
Management of Babies and Infants
The management of babies and infants with Great Vessels Transposition requires a multidisciplinary approach involving pediatricians, cardiologists, and specialized healthcare providers. Close monitoring of growth, development, and cardiac function is essential to address the unique needs of these young patients. Providing comprehensive care that includes regular check-ups, diagnostic evaluations, and early intervention strategies is crucial for optimizing outcomes and quality of life. Educating caregivers on recognizing potential symptoms and promoting a supportive environment for infants with this complex congenital heart defect is paramount. Collaborative efforts among healthcare professionals and families play a pivotal role in ensuring the well-being and long-term health of babies and infants with Great Vessels Transposition.
Role of Pediatricians in Care and Monitoring
Pediatricians play a crucial role in the care and monitoring of infants with Great Vessels Transposition. They are responsible for the initial evaluation, early detection of symptoms, and coordination of diagnostic tests to assess the infant’s cardiac health. Pediatricians work collaboratively with cardiologists to develop comprehensive treatment plans tailored to each baby’s specific needs. Regular follow-up visits, growth assessments, and developmental screenings are integral parts of pediatricians’ responsibilities in ensuring optimal health outcomes for infants with this congenital heart defect. Their expertise in child healthcare and ongoing monitoring are instrumental in managing the complexities of Great Vessels Transposition and supporting the overall well-being of affected infants.
Involvement of Cardiologists in Treatment
Cardiologists play a pivotal role in the treatment of Great Vessels Transposition, providing expertise in diagnosing and managing complex heart conditions. Their involvement includes performing specialized cardiac evaluations, interpreting diagnostic tests, and recommending appropriate interventions to address abnormal blood flow and oxygenation issues. Cardiologists collaborate closely with pediatricians and cardiac surgeons to create individualized care plans for infants with this congenital heart defect. Their in-depth knowledge of cardiovascular health and therapeutic options ensures comprehensive and effective treatment strategies that aim to improve outcomes and long-term prognosis for infants with Great Vessels Transposition. Cardiologists’ expertise is instrumental in guiding the medical management and surgical interventions necessary for the optimal care of these young patients.
Prognosis and Survival Rates
The prognosis and survival rates for individuals with Great Vessels Transposition have significantly improved due to advancements in medical care and surgical techniques. Early diagnosis, prompt intervention, and comprehensive management have contributed to better outcomes for affected individuals. Surgical procedures, such as the arterial switch operation, have shown high success rates in correcting the cardiac defects associated with this condition. Long-term follow-up care, lifestyle adjustments, and monitoring for potential complications are essential for ensuring the ongoing health and well-being of individuals with Great Vessels Transposition. Collaborative efforts among healthcare professionals and continuous advancements in treatment modalities continue to enhance the prognosis and long-term survival rates for patients with this complex congenital heart defect.
Outcomes of Surgical Procedures
Surgical procedures, such as arterial switch operations, have shown favorable outcomes in correcting the anatomical anomalies associated with Great Vessels Transposition. These interventions aim to restore normal blood flow patterns, optimize oxygenation, and improve cardiac function. Success rates for surgical correction of this congenital heart defect are high, with many infants demonstrating significant improvement in overall health and well-being postoperatively. Close post-surgical monitoring and rehabilitation play a crucial role in ensuring the successful recovery and long-term outcomes of individuals undergoing surgical intervention for Great Vessels Transposition. Continued research and advancements in surgical techniques further contribute to enhanced outcomes and a positive prognosis for patients with this complex cardiac condition.
Long-term Effects on Quality of Life
The long-term effects on the quality of life for individuals with Great Vessels Transposition can vary depending on factors such as the severity of the condition, the success of surgical interventions, and the presence of any complications. While many patients lead fulfilling lives after appropriate treatment, some may experience ongoing challenges related to cardiac function, exercise tolerance, or developmental delays. Multidisciplinary care involving cardiologists, pediatricians, and support services is essential in addressing the unique needs of individuals with this congenital heart defect throughout their lifespan. Monitoring for potential long-term complications, promoting healthy lifestyle choices, and providing ongoing medical support are essential components of improving the quality of life and overall well-being for those living with Great Vessels Transposition.