Disease ⏤ Diabetic Angiopathy
VII. Preventive Measures and Treatment Options
VIII. Management of Diabetic Angiopathy
I. Introduction to Diabetic Angiopathy
Diabetic Angiopathy, a serious complication of diabetes, refers to the damage that occurs to blood vessels due to prolonged high blood sugar levels. This condition is characterized by changes in the structure and function of blood vessels throughout the body. The vascular system, including arteries, veins, and capillaries, is adversely affected, leading to various complications.
Individuals with diabetes are at an increased risk of developing diabetic angiopathy, which can impact multiple organs and systems. The prolonged elevation of blood glucose levels in diabetes contributes to the development and progression of angiopathy. Understanding the mechanisms underlying this condition is crucial for effective management and prevention of its complications.
Diabetic angiopathy primarily affects small and large blood vessels, impairing blood circulation and causing damage to vital organs such as the eyes, kidneys, heart, and nerves. The intricate network of blood vessels throughout the body plays a critical role in maintaining proper function and health. Any disruption in vascular integrity due to diabetes can result in severe consequences.
By exploring the pathophysiology of diabetic angiopathy and its impact on different organ systems, healthcare professionals can tailor treatment strategies to address specific manifestations of this condition. Early detection and intervention are essential in mitigating the progression of diabetic angiopathy and reducing the associated risks of complications.
Throughout this article, we will delve into the complexities of diabetic angiopathy, from its effects on blood vessels to the intricate mechanisms of damage that occur in various organs. Understanding the role of blood vessels in this condition is key to elucidating the profound impact of diabetes on vascular health and overall well-being.
II. Understanding the Role of Blood Vessels
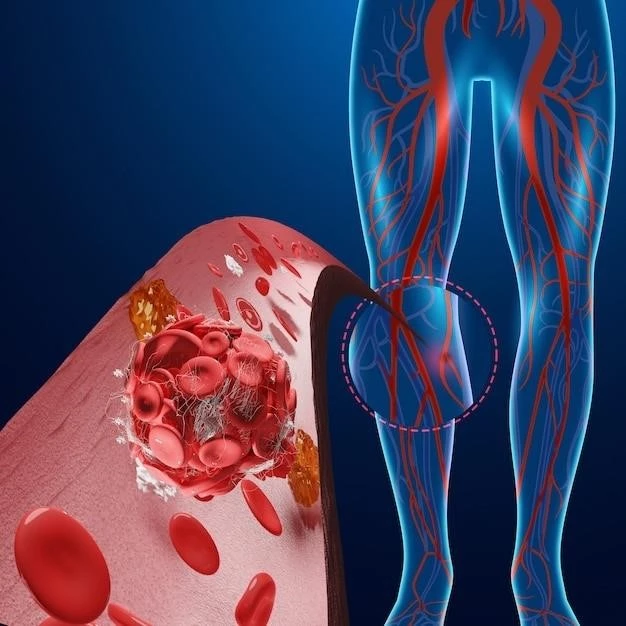
Blood vessels play a crucial role in the human body, serving as the intricate network responsible for transporting oxygen-rich blood, nutrients, and immune cells to various tissues and organs. In the context of diabetic angiopathy, the structural and functional integrity of blood vessels is significantly compromised due to the damaging effects of prolonged hyperglycemia.
Arteries, veins, and capillaries constitute the vascular system, with each vessel type playing a distinct role in maintaining proper circulation. Arteries carry oxygenated blood away from the heart to nourish tissues, veins return deoxygenated blood back to the heart, while capillaries facilitate nutrient and gas exchange at the cellular level. Any disruption in this delicate balance can lead to serious consequences.
In diabetes, persistent high levels of glucose in the bloodstream can trigger a cascade of events that contribute to vascular damage. The endothelial cells lining the blood vessels become dysfunctional, leading to inflammation and increased permeability. This not only hinders the smooth flow of blood but also promotes the accumulation of atherosclerotic plaques, further impeding circulation.
The altered vascular environment in diabetic angiopathy creates a state of chronic inflammation, perpetuating the cycle of damage to blood vessels. As a result, individuals with diabetes are more prone to developing conditions such as atherosclerosis, peripheral artery disease, and microvascular complications that affect organs like the eyes and kidneys.
Understanding the intricate interplay between hyperglycemia, endothelial dysfunction, inflammation, and vascular complications is essential in effectively managing diabetic angiopathy. By targeting specific pathways involved in vascular damage, healthcare providers can implement tailored interventions to preserve vascular health and minimize the risk of severe complications in patients with diabetes.
III. Impact on Eyes and Kidneys
Diabetic angiopathy exerts a significant impact on the eyes and kidneys, leading to potentially vision-threatening and renal complications in individuals with diabetes. The microvasculature in these organs is particularly vulnerable to the damaging effects of prolonged hyperglycemia, resulting in a spectrum of diabetic retinopathy and diabetic nephropathy.
In the eyes, the intricate network of blood vessels supplying the retina can be adversely affected by diabetic angiopathy. Changes in retinal blood flow and vascular permeability can lead to the development of diabetic retinopathy, a condition characterized by microaneurysms, hemorrhages, and abnormal vessel growth. Left untreated, diabetic retinopathy can progress to severe vision impairment and even blindness.
Similarly, the kidneys are highly vascular organs that play a crucial role in filtering waste products from the blood. In diabetic nephropathy, damage to the renal blood vessels due to diabetic angiopathy impairs the kidney’s filtration function, leading to the accumulation of waste products and protein in the urine. Over time, this can progress to chronic kidney disease and end-stage renal failure.
The impact of diabetic angiopathy on the eyes and kidneys underscores the systemic nature of vascular complications in diabetes. The shared pathogenesis of microvascular damage in these organs highlights the importance of early detection, regular screening, and optimal glycemic control to prevent or delay the progression of complications.
Healthcare providers must emphasize the significance of routine eye examinations and kidney function tests in individuals with diabetes to identify and address early signs of diabetic retinopathy and nephropathy. By closely monitoring vascular health in the eyes and kidneys, proactive interventions can be implemented to preserve vision and renal function, ultimately improving the quality of life for patients with diabetic angiopathy.
IV. Effects on the Heart and Nerves
Diabetic angiopathy can have profound effects on the heart and nerves, posing significant risks for cardiovascular disease and neuropathic complications in individuals with diabetes. The intricate network of blood vessels supplying the heart and nerves is susceptible to the damaging effects of prolonged hyperglycemia, leading to a range of cardiovascular and neurological manifestations.
In the heart, the coronary arteries that supply oxygenated blood to the cardiac muscle can be impacted by diabetic angiopathy. The narrowing of coronary vessels due to atherosclerosis and endothelial dysfunction can increase the risk of myocardial infarction and other cardiovascular events. Individuals with diabetes are more likely to develop coronary artery disease, which can have serious implications for heart health.
Furthermore, diabetic angiopathy can affect the autonomic and peripheral nerves, resulting in diabetic neuropathy. Nerve damage caused by impaired blood flow and inflammation can lead to symptoms such as pain, numbness, and tingling in the extremities. In severe cases, diabetic neuropathy can cause foot ulcers, infections, and even limb amputations.
Understanding the impact of diabetic angiopathy on the heart and nerves is crucial in implementing targeted interventions to mitigate the risks of cardiovascular disease and neuropathic complications. By addressing the underlying vascular changes and optimizing glycemic control, healthcare providers can help reduce the burden of heart-related issues and nerve damage in patients with diabetes.
Educating individuals with diabetes about the importance of cardiovascular health and nerve function is essential in promoting overall well-being and quality of life. Regular monitoring of heart function, blood pressure, and nerve sensitivity can aid in early detection and management of complications associated with diabetic angiopathy. Through a multidisciplinary approach, healthcare teams can collaborate to provide comprehensive care for patients affected by cardiovascular and neurological effects of diabetes.
V. Mechanisms of Damage
The mechanisms underlying the damage in diabetic angiopathy are multifactorial and involve complex interactions between hyperglycemia, inflammation, oxidative stress, and endothelial dysfunction. Prolonged exposure to elevated blood glucose levels initiates a cascade of events that contribute to the structural and functional abnormalities seen in blood vessels across various organ systems.
One of the key mechanisms of damage in diabetic angiopathy is endothelial dysfunction, where the endothelial cells lining the blood vessels exhibit impaired vasodilation, increased permeability, and pro-inflammatory properties. This dysfunctional endothelium promotes the adhesion of immune cells, formation of atherosclerotic plaques, and disruptions in blood flow regulation.
Chronic hyperglycemia also leads to the accumulation of advanced glycation end products (AGEs) within the blood vessels, contributing to increased oxidative stress and inflammation. AGEs promote the cross-linking of proteins, alter cellular signaling pathways, and induce the production of reactive oxygen species, all of which can further exacerbate vascular damage.
Inflammation plays a pivotal role in the pathogenesis of diabetic angiopathy, with pro-inflammatory cytokines and chemokines contributing to the recruitment of immune cells and amplification of vascular injury. The inflammatory milieu within blood vessels perpetuates a state of chronic inflammation that accelerates the progression of atherosclerosis and microvascular complications.
Moreover, alterations in the nitric oxide pathway, increased production of vasoconstrictors, and dysregulation of angiogenic factors further disrupt the delicate balance of vascular homeostasis in diabetic angiopathy. These changes not only impair blood flow but also exacerbate the susceptibility of blood vessels to additional insults, predisposing individuals with diabetes to a higher risk of cardiovascular events and organ damage.
By elucidating the intricate mechanisms of damage involved in diabetic angiopathy, researchers and healthcare providers can identify novel therapeutic targets and develop personalized treatment approaches to mitigate the vascular complications associated with diabetes. Strategies aimed at restoring vascular homeostasis, reducing inflammation, and improving endothelial function are essential in managing the complexities of diabetic angiopathy and enhancing the overall vascular health of individuals with diabetes.
VI. Risks and Complications Associated with Diabetic Angiopathy
Diabetic angiopathy poses a multitude of risks and complications for individuals with diabetes, significantly impacting their overall health and well-being. The systemic nature of vascular damage in diabetic angiopathy can lead to a variety of adverse outcomes, ranging from microvascular complications to macrovascular diseases.
Individuals with diabetes are at an increased risk of developing diabetic retinopathy, a condition characterized by damage to the blood vessels in the retina, which can lead to vision impairment and blindness if left untreated. Diabetic nephropathy, another common complication, is marked by kidney damage due to impaired blood flow, resulting in chronic kidney disease and renal failure.
Cardiovascular complications are also prevalent in diabetic angiopathy, with individuals facing a higher risk of coronary artery disease, heart attacks, and stroke. The narrowing and stiffening of blood vessels in diabetes contribute to poor circulation, elevated blood pressure, and an increased likelihood of developing heart-related problems.
In addition to the impact on the eyes, kidneys, and heart, diabetic angiopathy can result in peripheral artery disease, affecting blood flow to the limbs and increasing the risk of complications such as non-healing ulcers and lower limb amputations. Furthermore, the autonomic and peripheral nerves can be damaged, leading to diabetic neuropathy characterized by pain, numbness, and loss of sensation in the extremities.
Managing the risks and complications associated with diabetic angiopathy requires a comprehensive approach that focuses on optimizing glycemic control, controlling blood pressure and cholesterol levels, and adopting a healthy lifestyle. Regular monitoring of vascular health, kidney function, and nerve sensitivity is essential in early detection and timely intervention to prevent the progression of complications.
Educating individuals with diabetes about the potential risks and complications of diabetic angiopathy empowers them to take an active role in their health management. By promoting awareness, adherence to medical regimens, and lifestyle modifications, healthcare providers can help mitigate the impact of diabetic angiopathy and improve the long-term outcomes for patients with diabetes.
IX. Conclusion
In conclusion, diabetic angiopathy represents a complex and multifaceted complication of diabetes characterized by the detrimental effects on blood vessels throughout the body. The interplay of hyperglycemia, inflammation, oxidative stress, and endothelial dysfunction contributes to the structural and functional damage observed in various organ systems.
The impact of diabetic angiopathy extends beyond vascular complications, encompassing a wide array of risks and adverse outcomes such as diabetic retinopathy, diabetic nephropathy, cardiovascular diseases, and neuropathic complications. The systemic nature of this condition underscores the importance of early detection, continuous monitoring, and targeted interventions to prevent the progression of complications.
By understanding the mechanisms of damage underlying diabetic angiopathy and the intricate role of blood vessels in this process, healthcare providers can tailor treatment strategies to address specific manifestations of the disease. Emphasizing the importance of glycemic control, lifestyle modifications, and regular screenings is paramount in managing the risks associated with diabetic angiopathy.
Efforts to optimize vascular health, preserve organ function, and enhance overall well-being in individuals with diabetes are essential in mitigating the impact of diabetic angiopathy. Through a comprehensive and patient-centered approach, healthcare teams can collaborate to provide personalized care and support to individuals affected by this complex vascular complication.
Ultimately, the management of diabetic angiopathy requires a concerted effort to address the underlying mechanisms of damage, minimize risk factors, and prevent complications. By promoting awareness, education, and adherence to treatment regimens, healthcare professionals can empower individuals with diabetes to lead healthier lives and reduce the burden of diabetic angiopathy on their long-term health outcomes.