Overview of Intracranial Arteriovenous Malformations (AVMs)
Arteriovenous Malformations are abnormal tangles of blood vessels in the brain, potentially leading to serious neurological issues.
Definition and Introduction
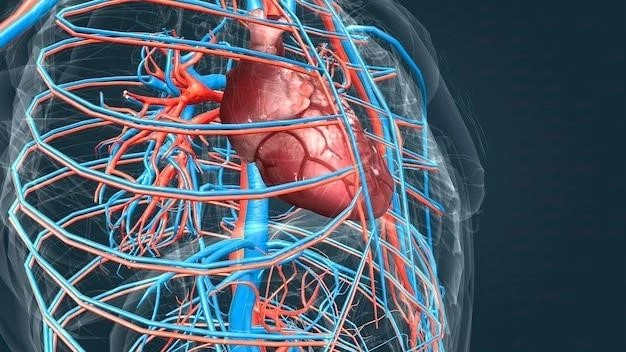
Arteriovenous Malformations in the brain are abnormal connections between arteries and veins without typical capillary beds. This direct connection disrupts normal blood flow patterns and can lead to various complications due to the high-pressure environment within these malformations. It is crucial to diagnose and treat these anomalies promptly to prevent potential neurological deficits and life-threatening complications.
Types of AVMs in the Brain
There are three main types of Intracranial Arteriovenous Malformations (AVMs) based on their feeding arteries⁚ superficial, deep, and pial. Superficial AVMs are located close to the brain’s surface, while deep AVMs reside in deeper brain regions. Pial AVMs involve the brain’s covering, the pia mater. Each type presents unique challenges and considerations in diagnosis and treatment, highlighting the complexity of managing these cerebrovascular anomalies.
Causes and Development of Intracranial AVMs
Arteriovenous Malformations in the brain result from abnormal connections between arteries and veins during fetal development.
Cerebral Blood Vessels Involvement
Intracranial Arteriovenous Malformations involve abnormal connections between arteries and veins in the brain, bypassing the usual capillary system. This direct connection disrupts the normal blood flow pattern, creating a risk for hemorrhage and other complications due to the malformation’s fragile structure. These anomalies can vary in size and location within the brain, influencing the potential symptoms and treatment options available.
Abnormal Formation of AVMs
The abnormal formation of Intracranial Arteriovenous Malformations occurs during embryonic development when blood vessels do not form correctly, resulting in direct connections between arteries and veins without the usual capillary network. This abnormality disrupts the natural blood flow regulation, leading to a high-pressure environment within the malformation. The complex interplay of genetic and environmental factors contributes to the development of these cerebrovascular anomalies, necessitating comprehensive treatment strategies tailored to each patient’s unique condition.
Symptoms and Diagnosis of Intracranial AVMs
Diagnosing Intracranial Arteriovenous Malformations involves identifying neurological symptoms and utilizing various diagnostic techniques.
Neurological Symptoms
Neurological symptoms associated with Intracranial Arteriovenous Malformations vary depending on the location and size of the malformation. Common symptoms include headaches, seizures, focal neurological deficits, visual disturbances, and cognitive impairment. The presentation of symptoms can be diverse, reflecting the complex nature of these cerebrovascular anomalies. Early recognition and prompt evaluation of neurological symptoms are crucial to facilitate timely diagnosis and appropriate management of Intracranial AVMs.
Diagnostic Techniques for Identifying AVMs
Various diagnostic techniques are employed to identify Intracranial Arteriovenous Malformations, including imaging studies such as MRI scans, CT angiography, and cerebral angiography. These imaging modalities help visualize the abnormal blood vessel connections, determine the AVM’s size and location, and assess the risk of potential complications. Additionally, neurological evaluations and specialized tests may be conducted to evaluate the patient’s symptoms and neurological function accurately. A comprehensive diagnostic approach is essential for creating an optimal treatment plan tailored to the individual’s specific AVM characteristics.
Treatment Options for Intracranial AVMs
Managing Intracranial Arteriovenous Malformations involves various treatment modalities to address the abnormal blood vessel connections effectively.
Surgical Interventions
Surgical interventions are a primary treatment option for Intracranial Arteriovenous Malformations. Procedures such as microsurgical resection aim to remove the abnormal blood vessel tangles while preserving surrounding brain tissue. Craniotomy and endovascular techniques may be utilized to access and treat the AVM, reducing the risk of hemorrhage and alleviating associated symptoms. Surgical interventions require a highly skilled neurosurgical team to ensure the best possible outcomes for patients with these complex cerebrovascular anomalies.
Radiosurgery and Embolization
Radiosurgery and embolization are non-invasive treatment options for Intracranial Arteriovenous Malformations. Radiosurgery, using focused radiation beams, aims to shrink the AVM over time. Embolization involves injecting glue or coils into the AVM to block blood flow, reducing the risk of rupture. These procedures are often used as standalone therapies or in combination with surgery to manage and reduce the size of the malformation, addressing the abnormal blood vessel connections while minimizing the risk of complications.
Complications Associated with Intracranial AVMs
Managing Intracranial Arteriovenous Malformations involves addressing potential hemorrhages and neurological deficits resulting from the abnormal blood vessel connections.
Hemorrhage and Neurological Deficits
Hemorrhage is a severe complication of Intracranial Arteriovenous Malformations, as the abnormal blood vessel connections can rupture, leading to bleeding in the brain. This can result in life-threatening consequences, including neurological deficits such as weakness, numbness, speech difficulties, and loss of coordination. Early recognition of symptoms indicative of hemorrhage is crucial to prompt intervention and mitigation of potential neurological impairments associated with AVMs.
Seizures and Cognitive Impairment
Intracranial Arteriovenous Malformations can manifest as seizures and cognitive impairment due to the disruptions in normal brain function caused by the abnormal blood vessel connections. Seizures are a common neurological symptom associated with AVMs, affecting coordination and consciousness. Cognitive impairment can range from memory difficulties to changes in behavior and decision-making processes. Effective management of seizures and cognitive challenges involves a comprehensive approach that addresses the underlying cerebrovascular anomalies and their impact on brain function.
Therapy and Management of Intracranial AVMs
Effective management of Intracranial Arteriovenous Malformations involves a comprehensive therapeutic approach tailored to each patient’s unique condition.
Medications and Rehabilitation
Medications may be prescribed to manage symptoms associated with Intracranial Arteriovenous Malformations, such as seizures and headaches. Rehabilitation programs focusing on physical, speech, or occupational therapy can help patients regain lost functions and improve their quality of life. A multidisciplinary approach involving healthcare professionals from various specialties is essential to provide comprehensive care for individuals with AVMs, addressing both medical and rehabilitative needs to optimize patient outcomes and promote recovery.
Long-term Monitoring and Follow-up Care
Long-term care for individuals with Intracranial Arteriovenous Malformations involves regular monitoring to assess the AVM’s stability, potential growth, or recurrence. Follow-up appointments with neurologists, neuroradiologists, and neurosurgeons are crucial to evaluate treatment effectiveness and address any new symptoms or complications. Periodic imaging studies and neurological assessments play a vital role in tracking the AVM’s progression and adjusting the management plan as needed. Long-term monitoring aims to ensure optimal outcomes and enhance the overall quality of life for patients living with AVMs.