Introduction to Panniculitis
Panniculitis is a group of diseases characterized by inflammation of subcutaneous adipose tissue. The condition can result from various causes and is diagnosed through clinical evaluation and biopsy.
Panniculitis is characterized by inflammation of subcutaneous adipose tissue. It can manifest from various causes and is diagnosed through clinical evaluation and biopsy. The condition involves inflammatory nodules or plaques and presents with symptoms such as tender skin nodules and systemic signs like weight loss and fatigue.
Definition and Overview
Panniculitis is characterized by inflammation of subcutaneous adipose tissue. It can manifest from various causes and is diagnosed through clinical evaluation and biopsy. The condition involves inflammatory nodules or plaques and presents with symptoms such as tender skin nodules and systemic signs like weight loss and fatigue.
Panniculitis presents with a variety of subtypes, including those related to infections, external insults, malignancies, and inflammatory diseases. Each subtype has distinct characteristics, requiring specific diagnostic and treatment approaches based on the underlying cause.
Common Causes and Triggers
Panniculitis can be triggered by various factors such as infections, external insults, malignancies, and inflammatory diseases. Identifying the underlying cause is crucial for determining the appropriate treatment and management plan for the condition.
Overview of Different Subtypes
Panniculitis presents with various subtypes related to infections, external insults, malignancies, and inflammatory diseases, each requiring specific diagnostic and treatment approaches.
Identifying Signs and Manifestations
The most common signs of panniculitis include the presence of tender skin nodules, red plaques, and systemic symptoms like weight loss, fever, and fatigue. Diagnosis often involves evaluating these skin manifestations along with clinical history and biopsy results.
Diagnosing panniculitis requires a thorough clinical assessment to identify skin manifestations, systemic symptoms, and potential underlying causes. A detailed evaluation is crucial for accurate diagnosis and appropriate management.
Importance of Clinical Evaluation
Diagnosing panniculitis involves a comprehensive clinical assessment to identify skin manifestations, systemic symptoms, and potential underlying causes. A detailed evaluation is essential for an accurate diagnosis and the development of an appropriate management plan.
Role of Biopsy in Confirming Diagnosis
Biopsy plays a crucial role in confirming the diagnosis of panniculitis by providing histological insights into the inflammatory changes in the subcutaneous fat tissue. It helps differentiate between various subtypes and guides appropriate treatment strategies based on the underlying pathology.
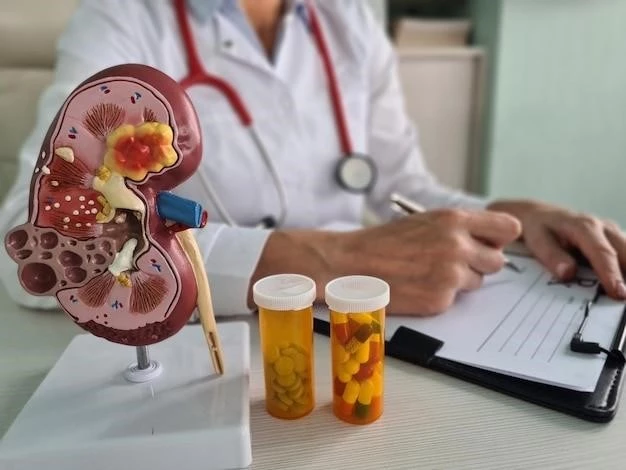
Medications Used in Management
Treatment of panniculitis may involve nonsteroidal anti-inflammatory drugs, antibiotics, or hydroxychloroquine based on the underlying cause.
Therapeutic Approaches and Lifestyle Changes
The treatment of panniculitis may involve medications such as nonsteroidal anti-inflammatory drugs, antibiotics, or hydroxychloroquine depending on the underlying cause. Additionally, lifestyle modifications such as adequate rest and proper nutrition may complement medical therapy in managing the condition.
Association with Pancreatic Disorders
Pancreatic panniculitis is a unique subset associated with pancreatic disorders such as acute and chronic pancreatitis, pancreatic carcinoma, and other malignancies. This specific form of panniculitis presents with distinct clinical features related to fat necrosis within the panniculus, often indicating an underlying pancreatic pathology.
Clinical Presentation and Unique Features
Pancreatic panniculitis manifests as lobular panniculitis with fat necrosis within the panniculus, often associated with pancreatic diseases like chronic pancreatitis or pancreatic cancer. This subset presents unique skin manifestations linked to underlying pancreatic malignancies.
Effects on Abdominal Fat Tissue
Mesenteric panniculitis primarily affects the adipose tissue within the mesentery, leading to chronic inflammation, fat necrosis, and eventual fibrosis. This condition poses diagnostic challenges due to its association with diverse etiologies and variable clinical presentations.
Mesenteric panniculitis, affecting the adipose tissue in the mesentery, presents diagnostic challenges due to its association with various etiologies. Chronic inflammation leading to fat necrosis and fibrosis characterizes this condition, emphasizing the importance of tailored diagnostic approaches for accurate identification and management.
Panniculitis can have complications such as scarring, chronic pain, and recurrent flare-ups. Prognosis varies depending on the subtype and underlying cause, with early diagnosis and appropriate treatment improving long-term outcomes.
Idiopathic nodular panniculitis is a rare skin disorder characterized by tender subcutaneous nodules or plaques that may be ulcerated. These nodules typically lead to inflammation in the subcutaneous fat tissue, distinguishing this condition from other types of panniculitis.
Idiopathic nodular panniculitis is a rare skin disorder characterized by tender subcutaneous nodules or plaques that may be ulcerated. These nodules typically lead to inflammation in the subcutaneous fat tissue, distinguishing this condition from other types of panniculitis.
Septal panniculitis refers to inflammation in the layer of fat tissue between the dermis and underlying fascia. Different forms, such as acute and chronic erythema nodosum, present various manifestations and diagnostic challenges, necessitating a detailed clinical approach for accurate management.
Popsicle panniculitis is a unique cold-induced inflammation that affects the subcutaneous tissue of the skin, commonly occurring in the cheeks due to exposure to cold. This condition involves inflammation in the lower skin layers triggered by exposure to cold temperatures, leading to distinctive skin manifestations.
Popsicle panniculitis is a unique cold-induced inflammation that affects the subcutaneous tissue of the skin, commonly occurring in the cheeks due to exposure to cold. This condition involves inflammation in the lower skin layers triggered by exposure to cold temperatures, leading to distinctive skin manifestations.
Septal panniculitis involves inflammation in the layer of fat tissue between the dermis and underlying fascia. Recognizing the specific forms such as acute and chronic erythema nodosum is essential for accurate diagnosis and tailored management approaches.
Forms and Clinical Considerations
Septal panniculitis involves inflammation in the layer of fat tissue between the dermis and underlying fascia. Recognizing the specific forms such as acute and chronic erythema nodosum is essential for accurate diagnosis and tailored management approaches.
Overview and Effects on Skin Layers
Popsicle panniculitis is a unique cold-induced inflammation that affects the subcutaneous tissue of the skin, commonly occurring in the cheeks due to exposure to cold. This condition involves inflammation in the lower skin layers triggered by exposure to cold temperatures, leading to distinctive skin manifestations.
Causes and Diagnostic Challenges
Idiopathic nodular panniculitis is a rare skin disorder characterized by tender subcutaneous nodules or plaques that may be ulcerated. This condition typically involves inflammation in the subcutaneous fat tissue, leading to diagnostic challenges due to its unique clinical presentation.
Potential Risks and Prognosis
Panniculitis can have complications such as scarring, chronic pain, and recurrent flare-ups. Prognosis varies depending on the subtype and underlying cause, with early diagnosis and appropriate treatment improving long-term outcomes.
Characteristics and Presentation
Popsicle panniculitis is a unique cold-induced inflammation affecting the skin’s subcutaneous tissue, typically seen in the cheeks due to exposure to cold temperatures. This distinct condition triggers inflammation in the lower skin layers, leading to specific skin manifestations.
