Introduction
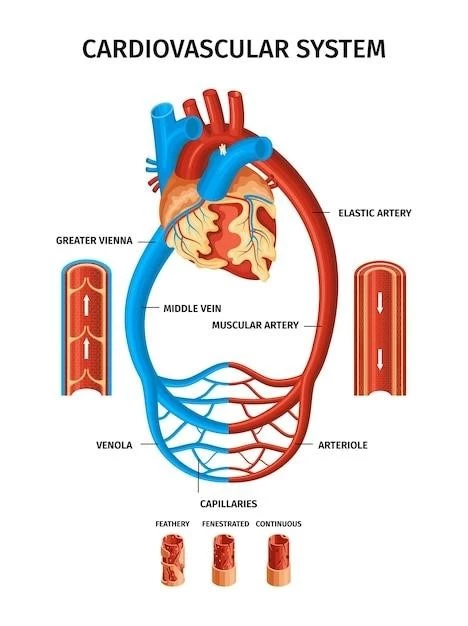
Persistent truncus arteriosus (TA) is a rare congenital heart defect where the heart’s single arterial trunk fails to divide into the pulmonary artery and aorta properly. This results in a single, large, arterial trunk that causes a mixture of oxygenated and deoxygenated blood circulation, impacting systemic, pulmonary, and coronary circulations.
Overview of Persistent Truncus Arteriosus
Persistent truncus arteriosus (TA) is a rare congenital heart defect where the heart’s single outflow artery fails to divide into the pulmonary artery and aorta as it should during fetal development. This results in a single, large arterial trunk that causes a mixture of oxygenated and deoxygenated blood circulation, impacting systemic, pulmonary, and coronary circulations. The condition often presents with a ventricular septal defect (VSD) and can lead to severe complications if left untreated. TA accounts for about 1% of congenital heart anomalies and 4% of critical congenital heart defects; It is crucial to diagnose and treat TA promptly to prevent potential life-threatening consequences. Various classification systems exist to categorize the different presentations of this complex cardiac anomaly.
Clinical Features
Persistent truncus arteriosus is characterized by a common arterial trunk, presence of a ventricular septal defect, and mixing of oxygenated and deoxygenated blood. Symptoms include cyanosis, heart failure signs, and abnormal heart sounds. Diagnosis involves physical exams, chest X-rays, ECGs, and echocardiography. Timely medical and surgical interventions are vital to manage the condition effectively.
Symptoms and Signs
Typical symptoms of persistent truncus arteriosus include cyanosis, heart failure signs, abnormal heart sounds, tachypnea, poor feeding, and diaphoresis. Patients may present with a hyperdynamic precordium, bounding pulses, a loud single S2 sound, a grade 2 to 4/6 systolic murmur, and an ejection sound. Diagnostic tests such as echocardiography, MRI, and CT angiography help confirm the diagnosis. Surgical repair is often necessary to manage the condition effectively and improve outcomes.
Classification
Collett and Edwards classification system categorizes Persistent truncus arteriosus into different types based on the configuration of the main pulmonary artery and the origins of the right and left pulmonary arteries from the truncus.
Collett and Edwards Classification
Collett and Edwards classification categorizes Persistent truncus arteriosus into different types based on the origin and division of the main pulmonary artery and the configuration of the right and left pulmonary arteries. The different types include Type I, Type II, Type III, Type A1, Type A2, Type A3, and Type A4, each describing specific patterns of the arterial trunk and the pulmonary arteries.
Diagnosis
Diagnosing persistent truncus arteriosus involves various methods, including physical exams, chest X-rays, ECGs, echocardiography, cardiac MRI, and CT angiography. These diagnostic tools help healthcare providers assess the heart’s structure and function, identify associated anomalies, and plan appropriate treatment strategies.
Diagnostic Methods
Diagnosis of persistent truncus arteriosus typically involves a combination of physical examination, chest X-rays, electrocardiograms (ECGs), echocardiography, cardiac MRI, and CT angiography. These diagnostic methods assist in confirming the presence of a large arterial trunk, assessing associated anomalies, and determining the best course of treatment for the condition. Early and accurate diagnosis is essential for appropriate management and improved outcomes in individuals with persistent truncus arteriosus.
Treatment
Persistent truncus arteriosus requires timely medical and surgical interventions. Medical management may include diuretics, digoxin, and angiotensin-converting enzyme inhibitors to manage heart failure before surgery. Surgical approaches involve repairing the ventricular septal defect, facilitating proper blood flow, and ensuring optimal cardiac function. Prostaglandin infusion may be used to maintain ductal patency in specific cases. Early surgical repair during the neonatal period is crucial for improved outcomes.
Medical Management
Medical management of persistent truncus arteriosus often involves the use of diuretics, digoxin, and angiotensin-converting enzyme (ACE) inhibitors to address heart failure symptoms before surgical intervention. Maintaining ductal patency with prostaglandin infusion may be necessary, especially in cases of interrupted aortic arch. Early surgical repair during the neonatal period is crucial for optimal outcomes and to correct the underlying cardiac anomalies effectively.
Surgical Approaches
Surgical management of persistent truncus arteriosus typically involves repairing the ventricular septal defect (VSD) and reconstructing the outflow tract to ensure improved blood flow and function. The procedure often includes closing the VSD, creating a conduit between the right ventricle and the pulmonary arteries, and addressing abnormalities of the truncal valve. Additionally, some surgical centers opt for non-conduit approaches using the patient’s own tissue to promote growth and minimize the need for future revisions. Branch pulmonary artery stenosis, a common complication, can be managed effectively with interventions like transcatheter balloon dilation with or without stent placement.

Complications
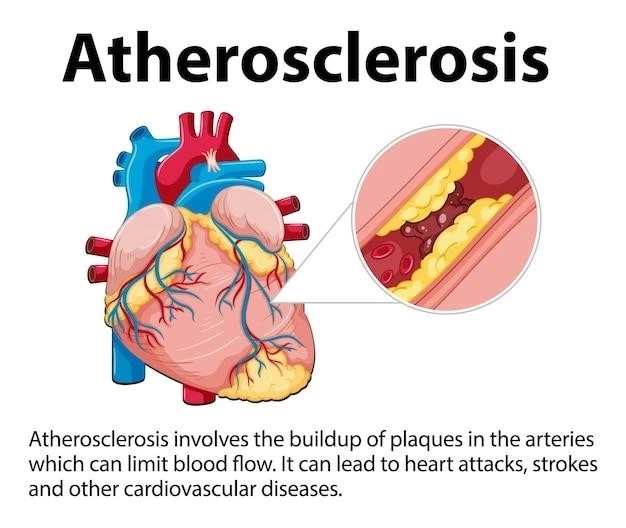
Persistent truncus arteriosus can lead to severe complications such as interrupted aortic arch, pulmonary hypertension, branch pulmonary artery stenosis, truncal valve abnormalities, and valve stenosis or regurgitation. These complications can impact heart function, circulation, and overall health, emphasizing the importance of timely diagnosis and appropriate management strategies to improve outcomes.
Associated Anomalies
Persistent truncus arteriosus is often associated with additional anomalies such as interrupted aortic arch, pulmonary hypertension, truncal valve abnormalities (stenosis or regurgitation), branch pulmonary artery stenosis, and septal defects. These conditions can further complicate the management of the heart defect and may require specific interventions to address each anomaly effectively. Early detection and comprehensive evaluation are crucial in identifying and managing these associated anomalies alongside persistent truncus arteriosus.
Prognosis
The prognosis for individuals with persistent truncus arteriosus depends on various factors, including the presence of associated anomalies, the timing of diagnosis, and the effectiveness of treatment. Early diagnosis and prompt surgical intervention significantly improve outcomes and reduce the risk of complications associated with this complex congenital heart defect. Long-term follow-up care is essential to monitor cardiac function, detect any potential issues early, and ensure optimal quality of life for affected individuals.
Outcomes and Follow-Up Care
The long-term outcomes for individuals with persistent truncus arteriosus depend on the timing of diagnosis, the success of surgical interventions, and the presence of associated anomalies. Early surgical repair significantly improves survival rates and quality of life. Follow-up care is essential to monitor cardiac function, detect any potential complications, and ensure ongoing management of the condition. Regular follow-up appointments, imaging studies, and cardiac evaluations help address any issues promptly and optimize the long-term prognosis for individuals living with persistent truncus arteriosus.