Introduction
Progressive external ophthalmoplegia is a clinical syndrome characterized by gradual ptosis and impaired eye mobility due to muscle weakness.
Overview of Progressive External Ophthalmoplegia
Progressive external ophthalmoplegia is a clinical syndrome characterized by gradual ptosis and impaired eye mobility due to muscle weakness. It can present as an isolated disorder or as part of a multisystemic syndrome and often involves mitochondrial dysfunction. The condition typically starts in adulthood and progresses over time, affecting the muscles responsible for eyelid and eye movement. Early recognition is crucial for optimal management of this rare genetic disease.
Causes and Types
Progressive external ophthalmoplegia can arise as an isolated disorder or as part of a multisystemic syndrome involving mitochondrial dysfunction, affecting muscle strength in the eyes and eyelids.
Chronic Progressive External Ophthalmoplegia Plus (CPEO Plus)
CPEO Plus, also known as Kearns-Sayre Syndrome (KSS)-spectrum, is a mitochondrial DNA deletion syndrome affecting the eyes and at least one other organ or system. This syndrome is characterized by symptoms beyond CPEO, typically occurring in individuals aged 20 or older.
Kearns-Sayre Syndrome (KSS)
Kearns-Sayre Syndrome (KSS) is a form of chronic progressive external ophthalmoplegia characterized by onset before the age of 20, bilateral ptosis, and pigmentary retinopathy. This syndrome is typically associated with additional conditions such as complete heart block and cerebrospinal fluid protein elevation, highlighting the multisystemic nature of the disorder.

Symptoms and Diagnosis
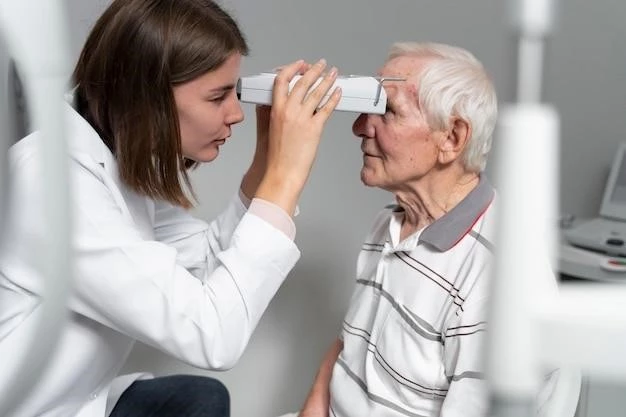
Chronic progressive external ophthalmoplegia presents with weakness of the eye muscles, bilateral ptosis, and limited eye movements. Symptoms typically manifest gradually and may vary in severity among individuals. Accurate diagnosis and monitoring are essential for managing this condition effectively.
Signs and Symptoms of Chronic Progressive External Ophthalmoplegia (CPEO)
Chronic progressive external ophthalmoplegia typically presents with weakness of the eye muscles, leading to bilateral ptosis (drooping eyelids), limited eye movements, and potentially other systemic manifestations of mitochondrial dysfunction. Patients may also experience increased fatigue and difficulty with activities requiring eye muscle strength, such as reading or driving. A thorough clinical evaluation and specialized testing are essential for accurately diagnosing CPEO.
Treatment and Management
Treatments for chronic progressive external ophthalmoplegia (CPEO) aim to manage symptoms such as ptosis and limited eye movements. Various approaches including physical therapy, corrective lenses, surgery, and medications can help improve quality of life for individuals with CPEO.
Treatments for Chronic Progressive External Ophthalmoplegia
Managing chronic progressive external ophthalmoplegia (CPEO) involves addressing symptoms like ptosis and limited eye movements. Treatment options may include physical therapy, surgery, specialized corrective lenses, and medications to improve quality of life for individuals affected by CPEO.
Prevalence and Incidence
Progressive external ophthalmoplegia (PEO) is a rare mitochondrial disorder with a prevalence rate of 11.5 cases per 100,000 individuals worldwide, highlighting its uncommon nature.
Global Prevalence of Chronic Progressive External Ophthalmoplegia (CPEO)
Chronic progressive external ophthalmoplegia (CPEO) is a rare mitochondrial disorder with a prevalence rate of 11.5 cases per 100٫000 individuals worldwide٫ underlining its infrequent occurrence.
Research and Studies
Advancements in the understanding of progressive external ophthalmoplegia have expanded knowledge on the diverse genetic and molecular underpinnings contributing to this condition, leading to improved diagnostic strategies and potential therapeutic interventions.
Advancements in the Understanding of Progressive External Ophthalmoplegia
Research on progressive external ophthalmoplegia has led to a deeper understanding of its genetic and molecular mechanisms, aiding in improved diagnostic techniques and potential therapeutic advancements for individuals affected by this condition.
Impact on Daily Life
Living with chronic progressive external ophthalmoplegia (CPEO) can present challenges due to muscle weakness affecting eye movements and eyelids. Coping strategies and support play vital roles in managing daily activities for individuals with CPEO.
Living with Chronic Progressive External Ophthalmoplegia (CPEO)
Individuals with chronic progressive external ophthalmoplegia (CPEO) face challenges related to muscle weakness affecting eye movements and eyelids, impacting daily activities like reading and driving. Coping mechanisms and a supportive environment are essential for managing the condition’s impact on daily life.
Complications and Prognosis
Potential complications associated with progressive external ophthalmoplegia include difficulties in daily activities due to eye muscle weakness, impacting quality of life. Prognosis varies but early diagnosis and appropriate management can improve outcomes.
Potential Complications Associated with Progressive External Ophthalmoplegia
Potential complications associated with progressive external ophthalmoplegia include difficulties in daily activities due to eye muscle weakness, impacting quality of life. Prognosis varies but early diagnosis and appropriate management can improve outcomes.
Future Directions
Emerging therapies and research areas for progressive external ophthalmoplegia focus on advancing diagnostic techniques and exploring potential therapeutic interventions to address the underlying genetic and molecular mechanisms contributing to this condition, aiming to enhance patient outcomes and quality of life.
Emerging Therapies and Research Areas for Progressive External Ophthalmoplegia
Ongoing research focuses on elucidating the genetic and molecular mechanisms underlying progressive external ophthalmoplegia, paving the way for innovative therapeutic approaches to address the root causes and improve outcomes for individuals with this challenging condition.
