Introduction
Disease⁚ Placenta neoplasm refers to the abnormal growths within the placenta, including choriocarcinoma and placental chorioangioma.
Overview of Placenta Neoplasm
Disease⁚ Placenta neoplasm encompasses various tumor-like conditions affecting the placenta, including choriocarcinoma, placental chorioangioma, and placental site trophoblastic tumor (PSTT).
Types of Placental Neoplasms
Placenta neoplasms include choriocarcinoma, placental chorioangioma, and placental site trophoblastic tumor (PSTT).
Choriocarcinoma
Choriocarcinoma is an aggressive malignancy of trophoblastic cells in the placenta, often arising after molar pregnancies or normal pregnancies. It is characterized by rapid growth and the potential to metastasize to distant sites.
Placental Chorioangioma
Placental chorioangioma, a common benign tumor originating from chorionic mesenchyme, is typically vascular and occurs in about 1 in pregnancies. While most chorioangiomas are small and clinically insignificant٫ larger ones may pose complications.
Placental Site Trophoblastic Tumor (PSTT)
Placental Site Trophoblastic Tumor (PSTT) is a rare gestational trophoblastic neoplasm originating from the placental implantation site. It was first recognized as trophoblastic pseudotumor and exhibits unique characteristics and behavior.
Pathophysiology of Placental Neoplasm
Placental neoplasms can originate from various placental tissues, exhibiting tumor-like characteristics and growth patterns.
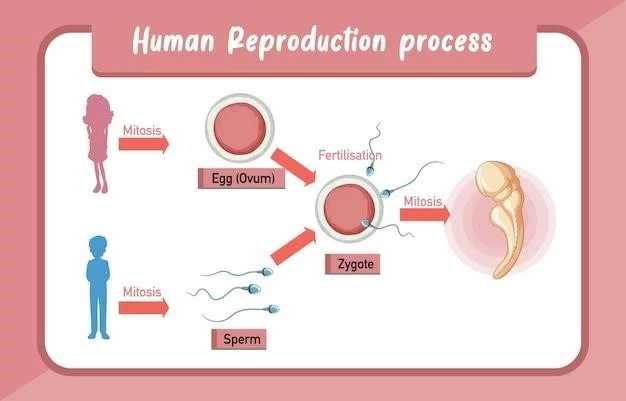
Tumor-like Behavior of the Placenta
The placenta exhibits tumor-like behavior in terms of invasion, growth patterns, and cellular characteristics, resembling neoplastic growth within the maternal-fetal interface.
Diagnosis and Management
Diagnosis of placenta neoplasms involves assessing tumor markers like serum human chorionic gonadotropin (hCG). Management includes chemotherapy and specific ICD coding for accurate classification.
Serum Human Chorionic Gonadotropin (hCG) as a Tumor Marker
Serum Human Chorionic Gonadotropin (hCG) serves as a crucial tumor marker for diagnosing placenta neoplasms due to its elevated levels in certain gestational trophoblastic diseases. It aids in monitoring response to treatment and disease progression.
ICD Coding for Placental Neoplasms
Accurate ICD coding for placental neoplasms is crucial for proper classification. Common codes include ICD-O⁚ 9100/3 for Choriocarcinoma, ICD-10⁚ C58 for Malignant neoplasm of placenta, and ICD-11⁚ 2C75 n XH8PK7 for Malignant neoplasms of placenta and choriocarcinoma, NOS.
Histopathological Features
Placental neoplasms present various histopathological features, including placental site nodules characterized by well-circumscribed nodular aggregates of trophoblastic cells within a hyalinized stroma.
Placental Site Nodules
Placental site nodules are characterized by well-circumscribed nodular aggregates of trophoblastic cells within a hyalinized stroma, showcasing distinct histopathological features in placental neoplasms.
Epidemiology and Incidence
Placenta neoplasms have varying incidences, with placental chorioangioma being a common benign tumor while placental site trophoblastic tumor is a rare gestational trophoblastic disease.
Prevalence and Associations
The prevalence of placenta neoplasms varies, with placental chorioangioma being a common benign tumor and placental site trophoblastic tumor (PSTT) being a rare gestational trophoblastic neoplasm with unique associations.
Clinical Presentations
Placenta neoplasms may present with varied clinical manifestations, including aggressive behavior and distinct characteristics related to tumor growth within the placenta.
Aggressive Behavior of Placental Neoplasms
Placental neoplasms may exhibit an aggressive nature characterized by rapid growth, invasion of surrounding tissues, and the potential for metastasis.
Treatment options for placenta neoplasms include chemotherapy, which is effective in managing gestational trophoblastic diseases such as choriocarcinoma and placental site trophoblastic tumors. Additionally, accurate ICD coding is essential for proper classification of these neoplasms.
Treatment Options
Chemotherapy is a primary treatment modality for managing gestational trophoblastic diseases like choriocarcinoma and placental site trophoblastic tumors. Accurate ICD coding is essential for proper classification of these neoplasms.
Radiological Findings
Radiological evaluations of placenta neoplasms may reveal characteristics such as placental lakes, reflecting pools of blood on scans indicating varying sizes and locations within the placenta.
Placental Lakes and Their Significance
Radiological findings in placenta neoplasms may include placental lakes, which are pools of blood visible on scans that can vary in size and location within the placenta, providing insights into the vascularization and structure of the placental tissue.
Research and Advances
Current research explores the link between oxygenation levels in the placenta and brain development, shedding light on potential impacts on fetal growth and long-term outcomes.
Oxygenation Levels in the Placenta and Brain Development
Research explores the impact of oxygenation levels in the placenta on fetal brain development, emphasizing the critical role of adequate oxygen supply for optimal neurodevelopment.
Prognosis and Outcomes
The prognosis of placenta neoplasms varies based on the specific type and stage, affecting long-term outcomes and potential cure rates for patients.
Cure Rates and Long-Term Effects
The cure rates and long-term outcomes for placenta neoplasms vary depending on the specific type, stage at diagnosis, and individual response to treatment, influencing the prognosis and quality of life for affected individuals.
Future Directions in Placental Neoplasm Studies
Further investigations will focus on exploring the relation between the placenta and cancer, delving into potential mechanisms driving tumorigenesis and therapeutic targets for placental neoplasms.
Exploration of the Link between Placenta and Cancer
Research focuses on investigating the connection between the placenta and cancer to understand potential mechanisms underlying tumorigenesis and therapeutic targets for placental neoplasms, aiming to improve diagnostic and treatment strategies in the future.
Case Studies and Clinical Insights
Updated diagnosis and management approaches for gestational trophoblastic diseases provide valuable insights into improving patient care and outcomes.
Update on the Diagnosis and Management of Gestational Trophoblastic Disease
Recent updates in diagnosing and managing gestational trophoblastic diseases provide crucial insights into enhancing patient care and treatment outcomes, reflecting advancements in the field.
Conclusion
As research continues to explore the link between placenta and cancer, advancements in understanding tumorigenesis and therapeutic targets for placental neoplasms pave the way for improved diagnostic and treatment strategies, offering hope for enhanced outcomes and care for affected individuals in the future.