Idiopathic Thrombocytopenic Purpura
Introduction
Welcome to the comprehensive guide on Idiopathic Immune Thrombocytopenic Purpura (ITP). This autoimmune disorder affects the platelet count, leading to a bleeding disorder due to improper blood clotting. In ITP, the immune system mistakenly targets and destroys platelets, the blood cells responsible for clotting. The presence of antibodies against platelets leads to their destruction mainly in the spleen but also in the liver and bone marrow. Understanding the underlying mechanisms of ITP is crucial for effective management. This guide aims to provide insights into the impact of ITP on the body, the diagnosis process, available treatment options such as corticosteroids and splenectomy, and ways to manage this condition on a daily basis. By delving into research advancements and offering practical tips for living with ITP, this guide will empower individuals affected by this disorder to navigate their journey with resilience and knowledge.
Understanding Blood Clotting
Understanding the process of blood clotting is essential in grasping the impact of Idiopathic Immune Thrombocytopenic Purpura (ITP). Blood clotting, or coagulation, is a complex cascade of events involving various blood components to stop bleeding. When a blood vessel is injured, platelets rush to the site to form a plug and stop the bleeding. Platelets, also known as thrombocytes, play a critical role in clot formation. In ITP, the reduced platelet count impedes the blood’s ability to clot effectively, increasing the risk of spontaneous bruising and petechiae. Delving into the nuances of how platelets interact with coagulation factors and blood vessel walls sheds light on why individuals with ITP are prone to bleeding episodes. By understanding the intricacies of blood clotting, individuals with ITP can gain insights into their condition and work closely with healthcare providers to optimize their treatment and management strategies.

Role of Antibodies
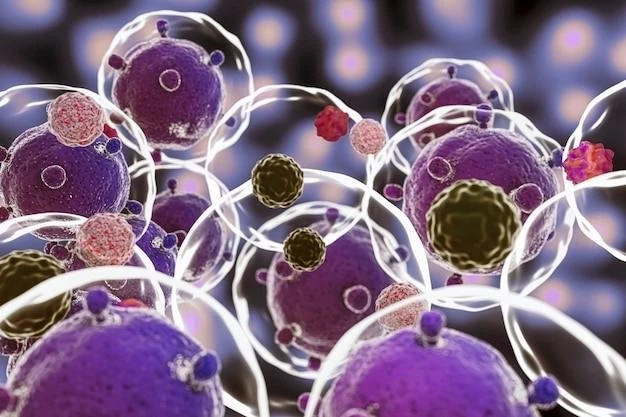
Antibodies play a pivotal role in the development of Idiopathic Immune Thrombocytopenic Purpura (ITP). In ITP, the immune system produces antibodies that target platelets, marking them for destruction by immune cells. These antibodies bind to platelets, leading to their premature removal from circulation and subsequent destruction primarily in the spleen. The presence of these antibodies triggers an immune response that results in a decreased platelet count, causing issues with blood clotting and increasing the risk of bleeding. Understanding the role of antibodies in ITP sheds light on the autoimmune nature of the disorder and underscores the importance of interventions that target the immune response to alleviate symptoms and prevent complications. By recognizing the impact of antibodies on platelet destruction, individuals with ITP can work proactively with healthcare providers to explore treatment options that address the underlying immune dysregulation.
Impact on Bone Marrow
The impact of Idiopathic Immune Thrombocytopenic Purpura (ITP) on bone marrow function is significant. In ITP, the immune system targets platelets for destruction, leading to a decrease in the platelet count. This reduction in platelets prompts the bone marrow to work overtime to produce more platelets to compensate for the ones being destroyed. The increased demand on the bone marrow can affect its normal function and lead to changes in the production of other blood cells. Monitoring the bone marrow’s response in ITP is crucial for understanding the body’s attempts to maintain adequate platelet levels despite ongoing destruction. By recognizing the impact on bone marrow function, healthcare providers can tailor treatment approaches to support bone marrow health while addressing the underlying immune dysregulation causing platelet destruction. Collaborating closely with healthcare teams can help individuals with ITP navigate the complexities of bone marrow involvement and optimize their management strategies for improved health outcomes.
Involvement of the Immune System
The involvement of the immune system in Idiopathic Immune Thrombocytopenic Purpura (ITP) is central to understanding this autoimmune disorder. In ITP, the immune system mistakenly produces antibodies that target platelets, marking them for destruction. This autoimmune response leads to a decrease in platelet count, impairing proper blood clotting function. The immune system’s role in ITP extends beyond platelet destruction, as immune dysregulation underlies the disorder’s pathophysiology. By recognizing the immune system’s involvement in ITP, individuals can explore treatments that aim to modulate the immune response and restore platelet levels. Collaborating with healthcare providers to address immune system dysfunction is key to managing ITP effectively. Understanding how the immune system contributes to ITP empowers individuals to advocate for tailored treatment approaches that target the root cause of the disorder, promoting better health outcomes and improved quality of life.
Symptoms⁚ Petechiae, Bruising, and Purpura
Recognizing the symptoms of Idiopathic Immune Thrombocytopenic Purpura (ITP) is crucial for early detection and management. Common symptoms of ITP include petechiae, which are small red or purple spots on the skin caused by minor bleeding under the skin. Additionally, individuals with ITP may experience easy bruising even with minimal trauma due to reduced platelet count affecting blood clotting. Purpura, larger purple patches on the skin, can also occur in ITP. Understanding these symptoms helps individuals with ITP monitor their health and seek timely medical intervention when needed. It is essential to track and report any unusual bruising, petechiae, or purpura to healthcare providers for proper evaluation and management. By staying vigilant and proactive about symptom recognition, individuals with ITP can work collaboratively with their healthcare team to optimize treatment strategies and improve overall well-being.
Diagnosis of ITP
Diagnosing Idiopathic Immune Thrombocytopenic Purpura (ITP) involves a comprehensive evaluation to confirm the underlying cause of a low platelet count. Healthcare providers may conduct a physical examination to look for characteristic signs such as petechiae and purpura. Blood tests, including a complete blood count (CBC) and a peripheral blood smear, can assess platelet levels and evaluate platelet morphology. In some cases, additional tests like bone marrow aspiration may be necessary to rule out other possible causes of thrombocytopenia. It’s essential for individuals experiencing symptoms of ITP, such as unexplained bruising or bleeding, to promptly seek medical attention for a proper diagnosis. By working closely with healthcare professionals and actively participating in the diagnostic process, individuals can gain clarity on their condition and begin personalized treatment to manage ITP effectively.
Treatment Options⁚ Corticosteroids
Corticosteroids are commonly used in the treatment of Idiopathic Immune Thrombocytopenic Purpura (ITP) to suppress the immune system’s attack on platelets. These medications work by reducing inflammation and decreasing antibody production, helping to increase platelet count and improve blood clotting. Prednisone is a frequently prescribed corticosteroid for ITP management. While corticosteroids can be effective in raising platelet levels, they may have side effects such as weight gain, mood changes, and increased risk of infections. It’s important for individuals undergoing corticosteroid treatment to closely follow their healthcare provider’s guidance, attend regular follow-up appointments, and report any concerning symptoms promptly. Collaborating with healthcare professionals to monitor treatment response and manage potential side effects optimizes the benefits of corticosteroid therapy in ITP. Seeking support and guidance throughout the treatment journey can help individuals navigate the use of corticosteroids effectively and enhance their overall well-being.
Treatment Options⁚ Splenectomy
Splenectomy, the surgical removal of the spleen, is a treatment option for some individuals with Idiopathic Immune Thrombocytopenic Purpura (ITP) who do not respond to other therapies. The spleen plays a key role in the destruction of platelets in ITP, so removing it can help increase platelet count and reduce the risk of bleeding. However, splenectomy is not without risks and considerations. After splenectomy, individuals may be at increased risk of certain infections, particularly those caused by encapsulated bacteria. Vaccinations against these organisms are often recommended before or after splenectomy to mitigate this risk. It’s crucial for individuals considering splenectomy to have detailed discussions with their healthcare team about the potential benefits, risks, and long-term implications of the procedure. Close post-operative monitoring and ongoing communication with healthcare providers are essential for optimizing outcomes and maintaining overall health following splenectomy as a treatment for ITP.
Management of ITP
Effective management of Idiopathic Immune Thrombocytopenic Purpura (ITP) involves a holistic approach that addresses symptoms, treatment strategies, and overall well-being. Regular monitoring of platelet counts and symptoms is essential to track the disease progression and treatment effectiveness. It’s important for individuals with ITP to maintain open communication with their healthcare team, report any new or worsening symptoms promptly, and actively participate in their care decisions. Embracing lifestyle modifications such as avoiding activities that may increase the risk of bleeding, adopting a balanced diet, and managing stress can contribute to improved health outcomes and quality of life. Support groups and educational resources can also provide valuable support and information for individuals living with ITP. By taking a proactive role in their health management, individuals with ITP can navigate the challenges of the condition with resilience and empower themselves to lead fulfilling lives despite the complexities of the disorder.
Research and Advancements
Ongoing research and advancements in the field of Idiopathic Immune Thrombocytopenic Purpura (ITP) offer hope for improved understanding and treatment options. Studies are investigating new therapies that target specific pathways involved in ITP pathophysiology, aiming to provide more targeted and effective interventions with fewer side effects. Advancements in diagnostic techniques and risk stratification help tailor treatment approaches to individual needs, enhancing personalized care for individuals with ITP. Clinical trials play a crucial role in evaluating novel treatments and expanding treatment options for ITP management. Keeping abreast of the latest research findings and participating in clinical trials when appropriate can offer individuals with ITP access to cutting-edge therapies and contribute to advancing the knowledge and management of the disorder. By staying informed about research initiatives and collaborating with healthcare providers to explore innovative treatments, individuals with ITP can actively engage in their care journey and potentially benefit from emerging advancements in the field.
Living with ITP
Living with Idiopathic Immune Thrombocytopenic Purpura (ITP) requires a proactive approach to managing the condition while maintaining overall well-being. It’s essential for individuals with ITP to educate themselves about the disorder, including its symptoms, treatment options, and potential complications. Engaging in open communication with healthcare providers, seeking support from loved ones, and connecting with patient advocacy groups can provide valuable resources and emotional support. Making lifestyle modifications such as engaging in regular physical activity, following a balanced diet rich in nutrients that support platelet production, and managing stress levels can positively impact health outcomes. Individuals with ITP should prioritize self-care, attend regular medical appointments, and adhere to treatment plans to optimize their overall health and quality of life. By building a strong support network, staying informed about the latest developments in ITP management, and taking an active role in their health, individuals with ITP can navigate the challenges of the condition with resilience and empowered self-care.
Conclusion
In conclusion, Idiopathic Immune Thrombocytopenic Purpura (ITP) poses unique challenges that require a comprehensive and patient-centered approach to management. By understanding the impact of ITP on blood clotting, the role of antibodies in platelet destruction, and the involvement of the immune system, individuals with ITP can work collaboratively with their healthcare team to tailor treatment strategies to their specific needs. Recognizing symptoms like petechiae, bruising, and purpura, seeking prompt diagnosis, and exploring treatment options such as corticosteroids and splenectomy are vital steps in managing ITP effectively. Embracing a holistic approach to care, staying informed about research advancements, and proactively engaging in self-care practices can empower individuals to lead fulfilling lives while managing the complexities of ITP. With ongoing support from healthcare providers, loved ones, and the broader community, individuals with ITP can navigate their journey with resilience, hope, and a commitment to their well-being.