Disease — Magnesium Wasting Renal
Magnesium wasting renal disease is a condition characterized by the body’s loss of magnesium through urine due to kidney dysfunction. This article will explore the role of magnesium in the body, symptoms of deficiency, causes of the disease, effects on kidney function, electrolyte imbalance, complications, treatment options, lifestyle changes, dietary adjustments, medication, therapies, and monitoring blood levels.
Introduction
Magnesium wasting renal disease is a serious medical condition that affects the kidneys’ ability to retain magnesium, leading to excessive loss of this essential electrolyte in the urine. Magnesium plays a crucial role in various bodily functions, including muscle and nerve function, blood glucose control, and blood pressure regulation.
Individuals with magnesium wasting renal disease may experience symptoms such as muscle cramps, weakness, tremors, fatigue, and abnormal heart rhythms due to magnesium deficiency. The causes of this disease can vary and may include genetic factors, medication side effects, or underlying kidney disorders.
Diagnosis of magnesium wasting renal disease involves assessing magnesium levels in the blood and urine, as well as evaluating kidney function through tests like creatinine clearance and glomerular filtration rate measurements. The disease can have profound effects on kidney function, leading to complications such as electrolyte imbalances, high blood pressure, and cardiovascular issues.
Treatment options for magnesium wasting renal disease focus on addressing the underlying kidney dysfunction and managing magnesium deficiency. Lifestyle changes, dietary adjustments, and medications may be recommended to help balance electrolyte levels and alleviate symptoms. Regular monitoring of blood magnesium levels is essential to track treatment effectiveness and adjust therapies as needed.
Understanding Renal Dysfunction
Renal dysfunction, specifically in the context of magnesium wasting renal disease, refers to the impaired ability of the kidneys to properly regulate magnesium levels in the body. The kidneys play a crucial role in filtering and reabsorbing minerals like magnesium to maintain the body’s electrolyte balance.
In cases of renal dysfunction, the renal tubules may malfunction, leading to increased excretion of magnesium in the urine. This results in a deficiency of magnesium in the bloodstream, which can have widespread effects on various bodily functions. The impaired reabsorption of magnesium by the kidneys contributes to the development of magnesium wasting renal disease.
Renal dysfunction can be caused by various factors, including chronic kidney disease, certain medications that affect renal function, genetic disorders affecting the kidneys, and other underlying health conditions. When the kidneys are not functioning optimally, electrolyte imbalances, including magnesium deficiency, can occur.
Understanding renal dysfunction is essential in the context of magnesium wasting renal disease as it sheds light on the mechanisms underlying the excessive loss of magnesium in the urine. Addressing renal dysfunction through targeted treatments and therapies is crucial in managing magnesium deficiency and improving overall kidney function in individuals affected by this disease.
Role of Magnesium in the Body
Magnesium is a vital mineral that plays diverse and essential roles in the human body. It is involved in over 300 enzymatic reactions, contributing to processes such as energy production, protein synthesis, muscle and nerve function, and DNA maintenance. Magnesium also plays a crucial role in regulating blood pressure, glucose levels, and the synthesis of neurotransmitters.
Within the cardiovascular system, magnesium helps maintain a steady heart rhythm and supports overall heart health. It plays a role in the relaxation of blood vessels, which can help lower blood pressure. In the muscular system, magnesium is necessary for muscle contraction and relaxation, making it important for physical performance and recovery.
Furthermore, magnesium is essential for maintaining healthy bones by promoting the synthesis of bone-forming cells and aiding in the regulation of calcium levels within the bone tissue. Magnesium also supports optimal immune function, helping the body defend against infections and diseases.
In individuals with magnesium wasting renal disease, the loss of magnesium through the urine can disrupt these vital functions, leading to symptoms of deficiency and various health complications. Understanding the importance of magnesium in the body highlights the significance of addressing magnesium deficiency in individuals with renal dysfunction to promote overall health and well-being.
Symptoms of Magnesium Deficiency
Magnesium deficiency can manifest in a variety of symptoms that impact overall health and well-being. Common signs of magnesium deficiency include muscle cramps, tremors, weakness, and fatigue due to its role in muscle function and energy metabolism. Individuals may also experience abnormal heart rhythms, dizziness, and nausea as magnesium is essential for heart health and nerve function.
Insufficient magnesium levels can affect mental health, leading to symptoms like irritability, anxiety, and depression, as magnesium plays a role in neurotransmitter regulation. Additionally, magnesium deficiency may impact bone health, contributing to an increased risk of osteoporosis and fractures.
Other symptoms of magnesium deficiency can include high blood pressure, fatigue, poor appetite, and numbness or tingling in the extremities. Severe magnesium deficiency can result in more serious complications such as seizures, personality changes, and cardiac arrhythmias.
In the context of magnesium wasting renal disease, where magnesium is lost through the urine due to kidney dysfunction, these symptoms of deficiency are particularly relevant. Recognizing and addressing the symptoms of magnesium deficiency is crucial in the diagnosis and management of magnesium wasting renal disease to prevent complications and improve the overall quality of life for affected individuals.
Causes of Magnesium Wasting Renal Disease
Magnesium wasting renal disease can have various underlying causes that contribute to the excessive loss of magnesium through the urine. One common cause is chronic kidney disease, where the kidneys’ ability to reabsorb magnesium is impaired, leading to its wastage. Inherited genetic disorders affecting renal tubule function can also result in magnesium wasting.
Certain medications and medical conditions can play a role in the development of magnesium wasting renal disease. Diuretics, often prescribed for conditions like high blood pressure or heart failure, can increase magnesium excretion by the kidneys, contributing to magnesium deficiency. Renal tubular acidosis, a condition that affects the kidney’s ability to maintain proper acid-base balance, can also lead to magnesium wasting.
Individuals with hyperparathyroidism, a condition characterized by overactive parathyroid glands, may experience magnesium wasting as elevated levels of parathyroid hormone can affect renal magnesium handling. Other factors such as alcoholism, malabsorption disorders, and certain cancers can also disrupt magnesium balance in the body and contribute to magnesium wasting renal disease.
Understanding the diverse causes of magnesium wasting renal disease is essential in diagnosing and managing the condition effectively. Identifying the underlying cause of magnesium loss through comprehensive evaluation and diagnostic testing is crucial in developing a targeted treatment plan to address both the renal dysfunction and magnesium deficiency in affected individuals.
Diagnosis of Magnesium Wasting Renal Disease
Diagnosing magnesium wasting renal disease involves assessing magnesium levels in the blood and urine to determine if there is excessive magnesium loss due to kidney dysfunction. Blood tests can reveal low magnesium levels, indicating deficiency, while urine tests can help quantify the amount of magnesium being excreted by the kidneys.
Additionally, evaluating kidney function through tests like creatinine clearance and glomerular filtration rate measurements is essential in diagnosing renal dysfunction associated with magnesium wasting. Imaging studies such as ultrasounds or CT scans may be performed to assess the structure and function of the kidneys and identify any underlying conditions that could be contributing to magnesium loss.
A thorough medical history review, including family history of kidney disorders and medication use, can provide valuable insights into potential causes of magnesium wasting renal disease. Symptoms such as muscle cramps, weakness, and abnormal heart rhythms may also be taken into consideration during the diagnostic process.
Diagnosing magnesium wasting renal disease requires a multidisciplinary approach involving nephrologists, endocrinologists, and other healthcare professionals. By conducting a comprehensive evaluation of magnesium levels, kidney function, and potential contributing factors, healthcare providers can accurately diagnose the condition and develop a personalized treatment plan to address magnesium deficiency and renal dysfunction effectively.
Effects on Kidney Function
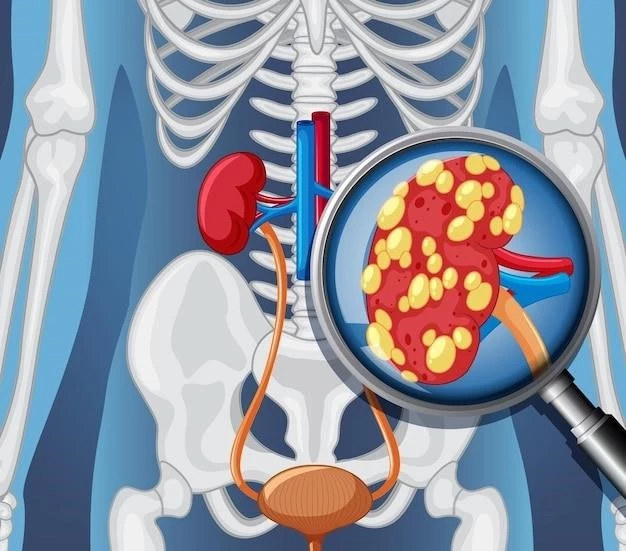
Magnesium wasting renal disease can have significant effects on kidney function, impacting the kidneys’ ability to properly regulate electrolyte balance and magnesium levels in the body. The excessive loss of magnesium through the urine due to renal dysfunction can lead to a range of complications affecting kidney health.
Impaired reabsorption of magnesium by the renal tubules can strain the kidneys and contribute to electrolyte imbalances, disrupting the delicate equilibrium necessary for optimal kidney function. This dysregulation of magnesium levels can further exacerbate renal dysfunction, leading to a vicious cycle of worsening kidney function and magnesium deficiency.
Chronic magnesium wasting can also damage the renal tubules over time, reducing their ability to effectively concentrate urine and maintain electrolyte balance. This can increase the risk of developing other kidney-related conditions, such as nephrocalcinosis or kidney stones, further compromising kidney function.
Moreover, the effects of magnesium wasting renal disease on kidney function can manifest as decreased renal reserve, impaired filtration capacity, and reduced ability to excrete waste products from the body. Over time, these effects can progress to more severe kidney impairment, potentially leading to chronic kidney disease or end-stage renal disease if left untreated.
Understanding the profound effects of magnesium wasting renal disease on kidney function underscores the importance of early detection and intervention to preserve renal health. By addressing magnesium deficiency, restoring electrolyte balance, and treating underlying renal dysfunction, healthcare providers can help mitigate the impact of this disease on the kidneys and improve overall kidney function in affected individuals.
Electrolyte Imbalance
Electrolyte imbalance is a significant concern in individuals with magnesium wasting renal disease, as the excessive loss of magnesium through the urine disrupts the body’s electrolyte equilibrium. Magnesium, alongside other electrolytes like potassium, sodium, and calcium, plays a crucial role in various physiological processes.
Renal dysfunction associated with magnesium wasting can lead to imbalances in multiple electrolytes, affecting the body’s ability to maintain proper fluid balance, nerve function, and muscle contractions. The dysregulation of magnesium levels, in particular, can impact the function of the heart, muscles, and nerves, leading to a range of symptoms.
Electrolyte imbalances resulting from magnesium wasting can manifest as muscle weakness, irregular heart rhythms, fatigue, and neuromuscular abnormalities. Potassium and calcium levels may also be affected, further exacerbating symptoms such as muscle cramps, cardiac arrhythmias, and bone demineralization.
Disruptions in electrolyte balance can have systemic effects on the body, potentially impacting organ function, nerve transmission, and overall health. Severe electrolyte imbalances can be life-threatening and require prompt intervention to restore equilibrium and prevent complications.
Managing electrolyte imbalance in individuals with magnesium wasting renal disease involves addressing deficiencies in magnesium and other electrolytes through targeted treatments and therapies. Regular monitoring of electrolyte levels, kidney function, and overall health status is essential to detect and manage imbalances early, optimizing outcomes and improving quality of life for affected individuals.
Complications Associated with the Disease
Magnesium wasting renal disease can lead to various complications that affect overall health and well-being. One of the primary complications of this disease is the development of severe magnesium deficiency, which can result in symptoms such as muscle weakness, cramps, and cardiac arrhythmias due to the crucial role of magnesium in muscle and heart function.
Chronic magnesium wasting can also lead to electrolyte imbalances, including disruptions in potassium and calcium levels, which may contribute to additional complications such as muscle spasms, fatigue, and bone disorders. These imbalances can further impact nerve function, cardiovascular health, and bone density, increasing the risk of fractures and related complications.
Furthermore, magnesium deficiency and electrolyte imbalances associated with magnesium wasting renal disease can have systemic effects on the body, leading to symptoms like dizziness, nausea, and mental health disturbances. Individuals may experience fatigue, irritability, and cognitive impairment as a result of inadequate magnesium levels impacting neurotransmitter function.
In severe cases, complications of magnesium wasting renal disease can include seizures, personality changes, and cardiac abnormalities. Prolonged magnesium deficiency and electrolyte imbalances can also contribute to the progression of kidney dysfunction, potentially leading to chronic kidney disease and end-stage renal failure if left untreated.
Understanding and managing the complications associated with magnesium wasting renal disease is crucial in preserving overall health and mitigating the risks of long-term complications. Early detection, intervention, and comprehensive treatment plans that address both magnesium deficiency and renal dysfunction are essential in improving outcomes and quality of life for individuals affected by this condition.
Treatment Options
Treating magnesium wasting renal disease involves addressing both the underlying renal dysfunction and magnesium deficiency to restore optimal kidney function and electrolyte balance. Treatment options may vary depending on the severity of the condition and the individual’s overall health status.
One key aspect of treatment is managing magnesium deficiency through oral magnesium supplements or intravenous administration in severe cases. By replenishing magnesium levels, healthcare providers aim to alleviate symptoms, support muscle and nerve function, and prevent complications associated with magnesium deficiency.
Addressing renal dysfunction is essential in managing magnesium wasting renal disease. This may involve medications to improve kidney function, control blood pressure, or treat underlying conditions contributing to kidney dysfunction. Lifestyle modifications such as maintaining a healthy diet, staying hydrated, and avoiding excessive alcohol consumption can also support kidney health.
In some cases, individuals with magnesium wasting renal disease may require dialysis or other renal replacement therapies to help maintain electrolyte balance and manage kidney function. These interventions can be essential for individuals with advanced kidney disease and severe complications related to magnesium deficiency.
Regular monitoring of kidney function, magnesium levels, and electrolyte balance is crucial in tracking treatment effectiveness and adjusting therapies as needed. Collaborating with a multidisciplinary healthcare team, including nephrologists, dietitians, and pharmacists, can help develop a comprehensive treatment plan tailored to the individual’s specific needs and health goals.
Lifestyle Changes
Implementing lifestyle changes is essential for individuals with magnesium wasting renal disease to support kidney health, manage electrolyte imbalances, and improve overall well-being. Adopting a healthy lifestyle can help optimize treatment outcomes and reduce the risk of complications associated with this condition.
One key lifestyle change is maintaining a balanced diet rich in magnesium-containing foods such as nuts, seeds, whole grains, leafy green vegetables, and fish. By incorporating magnesium-rich foods into your diet, you can help replenish magnesium levels and support essential bodily functions.
Staying hydrated by drinking an adequate amount of water each day is crucial for kidney health. Adequate hydration can help prevent kidney stone formation, support optimal kidney function, and facilitate the elimination of waste products from the body.
Avoiding excessive alcohol consumption is important as alcohol can impair kidney function and interfere with electrolyte balance. Moderating alcohol intake or abstaining from alcohol altogether can help protect kidney health and prevent further complications related to magnesium wasting renal disease.
Incorporating regular physical activity into your routine can promote overall health and help manage symptoms associated with magnesium deficiency. Exercise can support muscle strength, cardiovascular health, and mental well-being, contributing to a holistic approach to managing magnesium wasting renal disease.
Engaging in stress-reducing activities such as meditation, yoga, or mindfulness practices can also benefit individuals with magnesium wasting renal disease. Chronic stress can impact kidney function and exacerbate symptoms, so prioritizing stress management techniques can support both physical and mental health.
Dietary Adjustments
Dietary adjustments play a crucial role in managing magnesium wasting renal disease by supporting kidney function, replenishing magnesium levels, and maintaining electrolyte balance. Making strategic changes to your diet can help improve symptoms, prevent complications, and enhance overall health outcomes.
Focusing on foods that are rich in magnesium can help address deficiency in individuals with magnesium wasting renal disease. Incorporate magnesium sources like almonds, cashews, spinach, avocados, and whole grains into your meals to boost magnesium intake and support essential bodily functions.
Limiting sodium intake is important for individuals with magnesium wasting renal disease as excess sodium can contribute to fluid retention and high blood pressure, further impacting kidney health. Avoiding processed foods, salty snacks, and adding minimal salt to meals can help reduce sodium consumption.
Monitoring potassium intake is also crucial, especially if potassium levels are affected by magnesium loss. Consuming potassium-rich foods like bananas, sweet potatoes, oranges, and tomatoes in moderation can help maintain a healthy balance of electrolytes and support optimal kidney function.
Including adequate fiber in your diet from fruits, vegetables, whole grains, and legumes can support digestive health and promote regular bowel movements. Fiber can also help bind excess minerals in the gut, reducing the risk of mineral imbalances related to magnesium wasting renal disease.
Collaborating with a registered dietitian or healthcare provider to develop a personalized dietary plan tailored to your specific needs and health goals is essential. By making targeted dietary adjustments, individuals with magnesium wasting renal disease can optimize nutrition, support kidney function, and enhance overall well-being.
Medication and Therapies
Medication and therapies play a vital role in the treatment of magnesium wasting renal disease, targeting both renal dysfunction and magnesium deficiency to restore balance and support kidney function. Various medications and therapeutic approaches can help manage symptoms, address underlying causes, and improve overall health outcomes.
Supplementation with oral magnesium supplements is a common approach to replenishing magnesium levels in individuals with magnesium wasting renal disease. Healthcare providers may prescribe magnesium tablets or liquid formulations to help correct deficiencies and alleviate symptoms associated with magnesium deficiency.
Diuretics, medications that increase urine production, may be prescribed cautiously to manage fluid retention and control blood pressure in individuals with magnesium wasting renal disease. However, diuretics can also contribute to further magnesium loss, so monitoring electrolyte levels and kidney function is essential when using these medications.
Phosphate binders may be recommended to individuals with magnesium wasting renal disease to help manage phosphate levels in the body. These medications can prevent the absorption of dietary phosphate in the gut, reducing the risk of hyperphosphatemia and related complications that can arise from kidney dysfunction.
In cases of severe kidney dysfunction, renal replacement therapies such as dialysis may be necessary to support kidney function, remove waste products from the blood, and help maintain electrolyte balance. Dialysis can be a life-saving intervention for individuals with advanced kidney disease and severe magnesium wasting complications.
Collaborating with healthcare providers to determine the appropriate medications and therapies for your specific condition is crucial. By following prescribed treatment regimens, monitoring kidney function and electrolyte levels, and participating in therapeutic interventions, individuals with magnesium wasting renal disease can improve symptoms, prevent complications, and enhance their quality of life.
In conclusion, magnesium wasting renal disease poses significant challenges to kidney function and electrolyte balance, leading to magnesium deficiency and associated complications. Understanding the role of magnesium in the body, the effects of renal dysfunction, and the complexities of managing this condition is essential for healthcare providers and individuals affected by this disease.
Diagnosis of magnesium wasting renal disease requires comprehensive evaluation of magnesium levels, kidney function, and underlying causes to develop personalized treatment plans. Lifestyle changes, dietary adjustments, medication, and therapies play crucial roles in managing symptoms, restoring magnesium balance, and supporting kidney health.
Addressing complications associated with magnesium wasting renal disease, such as electrolyte imbalances and kidney dysfunction, requires a multidisciplinary approach and regular monitoring to optimize outcomes. Collaborating with healthcare providers, following prescribed treatment regimens, and making necessary lifestyle modifications are key steps in managing this condition effectively.
By implementing targeted interventions, individuals with magnesium wasting renal disease can mitigate symptoms, prevent long-term complications, and improve their overall quality of life. Through education, early intervention, and ongoing support, individuals can navigate the challenges of this disease and work towards better kidney health and well-being.