Understanding Biliary Atresia
Causes of Biliary Atresia
Biliary atresia is a rare condition with an unknown exact cause, though several factors are believed to contribute. Possible causes include genetic abnormalities, viral infections, immune system issues, and abnormalities during fetal development.
Genetic predisposition may play a role in some cases, as certain genes have been linked to an increased risk of biliary atresia. Viral infections, such as cytomegalovirus, have been researched for potential associations with the condition.
Immune system dysfunction is also considered a possible cause, where the body’s immune response mistakenly targets the bile ducts. Lastly, abnormalities during fetal development could lead to improper formation of the bile ducts, contributing to biliary atresia.
Symptoms of Intrahepatic Biliary Atresia
Intrahepatic biliary atresia presents a range of symptoms related to impaired bile flow from the liver. Early signs may include jaundice, dark urine, pale stools, and abdominal swelling. As the condition progresses, infants may experience poor weight gain, irritability, and persistent itching.
Due to the buildup of bile in the liver, affected individuals may develop liver damage, leading to complications such as cirrhosis. Timely diagnosis and intervention are crucial to manage symptoms and improve outcomes for patients with intrahepatic biliary atresia.
Treatment Options for Syndromic Biliary Atresia
Managing syndromic biliary atresia involves a multidisciplinary approach aimed at improving bile flow and supporting liver function. Treatment typically includes surgical intervention, such as the Kasai procedure, to restore bile flow. In cases where surgery is not feasible, liver transplantation may be considered.
Alongside invasive procedures, medical management focuses on symptom relief, nutritional support, and monitoring liver function. Regular follow-up care is essential to assess treatment response and address any potential complications that may arise.
Collaboration between healthcare providers, including hepatologists, surgeons, and nutritionists, is crucial in developing a comprehensive treatment plan tailored to the individual needs of patients with syndromic biliary atresia.
Prognosis for Biliary Atresia Patients
The prognosis for patients with biliary atresia varies depending on several factors, including the promptness of diagnosis, the effectiveness of treatment, and the presence of complications. Early detection and timely intervention, such as the Kasai procedure, can improve outcomes and potentially delay the need for liver transplantation.
Despite advancements in treatment, some individuals may eventually require a liver transplant due to progressive liver damage. Long-term prognosis post-transplantation is generally favorable, although ongoing medical management and monitoring are essential to ensure graft function and overall well-being.
It is important for healthcare providers to work closely with patients and their families to provide support, education, and comprehensive care throughout the disease course, optimizing the prognosis and quality of life for individuals affected by biliary atresia.
Surgical Interventions for Biliary Atresia
Surgical interventions play a crucial role in the management of biliary atresia, with the Kasai procedure being the primary surgical option for infants diagnosed with the condition. The Kasai procedure aims to establish bile flow by removing the damaged bile ducts and connecting the liver directly to the small intestine.
In cases where the Kasai procedure is not successful or when biliary atresia progresses to advanced stages, liver transplantation may be necessary. Liver transplantation offers a long-term solution for patients with end-stage liver disease resulting from biliary atresia, providing them with a chance for improved quality of life and overall survival.
Collaboration between pediatric surgeons, hepatologists, and transplant specialists is essential to ensure appropriate surgical management tailored to the individual needs of patients with biliary atresia.

Complications of Biliary Atresia
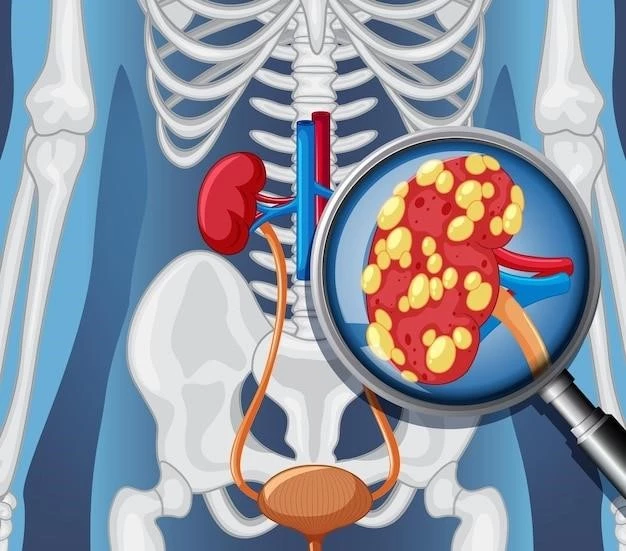
Biliary atresia can lead to various complications, primarily due to the obstruction of bile flow from the liver. Without proper drainage, bile accumulates and causes liver damage, leading to conditions such as cirrhosis and portal hypertension. These complications can progress to end-stage liver disease, requiring liver transplantation.
Other potential complications include cholangitis, a bacterial infection of the bile ducts, and malabsorption of essential nutrients due to impaired bile secretion. Individuals with biliary atresia may also experience growth delays, nutritional deficiencies, and an increased risk of developing hepatocellular carcinoma.
Managing complications associated with biliary atresia requires a comprehensive approach, including close monitoring of liver function, nutritional support, and timely interventions to address any arising issues and optimize long-term outcomes for affected individuals.
Research Updates on Intrahepatic Biliary Atresia
Ongoing research into intrahepatic biliary atresia focuses on understanding the underlying mechanisms of the disease, improving diagnostic methods, and exploring novel treatment approaches. Recent studies have delved into the genetic factors contributing to biliary atresia, potential biomarkers for early detection, and the role of the immune system in disease progression.
New research initiatives also aim to enhance surgical techniques, such as refining the Kasai procedure and exploring minimally invasive alternatives. Additionally, studies are investigating the impact of innovative therapies, including stem cell transplants and gene editing, on improving outcomes for patients with intrahepatic biliary atresia.
By advancing our knowledge of intrahepatic biliary atresia through ongoing research efforts, the medical community strives to develop more effective strategies for diagnosis, treatment, and long-term management, ultimately improving the quality of life for individuals affected by this challenging condition.
Support and Resources for Syndromic Biliary Atresia
Individuals and families affected by syndromic biliary atresia often require comprehensive support and access to various resources to navigate the challenges associated with the condition. Support networks, such as patient advocacy groups and online forums, offer valuable emotional support, information sharing, and community engagement for those impacted by biliary atresia.
Furthermore, healthcare providers play a crucial role in providing guidance, counseling, and coordination of care for individuals with syndromic biliary atresia. Specialized clinics, multidisciplinary teams, and social workers can assist in addressing the medical, educational, and psychosocial needs of patients and families throughout the disease journey.
Access to educational materials, financial assistance programs, and therapeutic services can also help enhance the well-being and quality of life of individuals with syndromic biliary atresia. By leveraging available support and resources, patients can better cope with the challenges of the condition and optimize their overall health outcomes.