Chronic necrotizing vasculitis is a serious condition characterized by the inflammation and destruction of blood vessels.
Overview of Chronic Necrotizing Vasculitis
Chronic necrotizing vasculitis involves the immune system mistakenly attacking blood vessels. Genetic predisposition, environmental factors, and certain infections are potential triggers. Understanding these underlying causes is crucial for effective management and treatment of this complex condition.
Potential Triggers and Risk Factors
The development of chronic necrotizing vasculitis can be influenced by various factors such as autoimmune disorders, exposure to certain chemicals, medications, or infections. Genetic susceptibility and environmental triggers play pivotal roles in the onset of this inflammatory condition.
Common Symptoms of Vasculitis
The symptoms of vasculitis may vary depending on the type and affected organs but can include fatigue, fever, weight loss, skin rashes, nerve problems, and organ-specific manifestations. Prompt recognition and diagnosis are essential for initiating appropriate treatment and preventing potential complications.
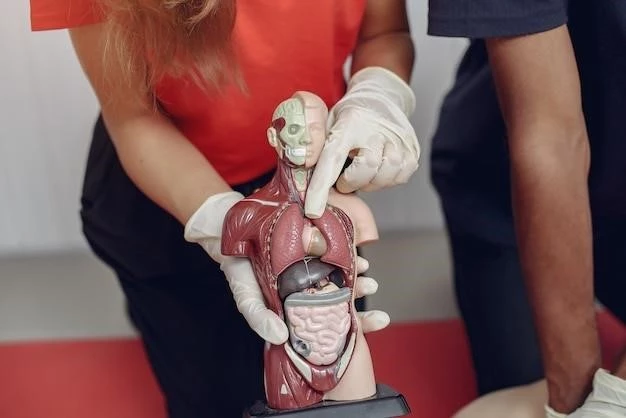
Diagnostic Procedures for Identifying Vasculitis
Diagnosing vasculitis often involves a combination of medical history review, physical examination, blood tests, imaging studies (such as angiography or MRI), and in some cases, a biopsy of affected tissue. These diagnostic procedures help confirm the presence of vasculitis, determine its severity, and guide appropriate treatment strategies.
Medication-Based Treatments

Medication-based treatments for necrotizing vasculitis may include immunosuppressants, corticosteroids, and biologic therapies. These medications aim to suppress the overactive immune response, reduce inflammation, and prevent further damage to blood vessels. Close monitoring by healthcare providers is essential to adjust dosages and manage potential side effects effectively.
Surgical Interventions for Severe Cases
In severe cases of necrotizing vasculitis, surgical interventions may be necessary to repair damaged blood vessels, remove affected tissue, or address complications such as aneurysms. Surgeries like vascular bypass procedures or angioplasty can help improve blood flow and reduce the risk of further vascular damage. Surgery is often reserved for cases where medication-based treatments are insufficient.
Strategies to Handle Flare-Ups
Strategies for managing chronic vasculitis flare-ups include adjusting medication dosages, rest, stress reduction techniques, and close monitoring of symptoms. Prompt communication with healthcare providers is crucial to address flare-ups effectively and prevent long-term complications. Patients should adhere to treatment plans and seek medical attention if symptoms worsen.
Importance of Regular Monitoring and Follow-Up Care
Regular monitoring and follow-up care are essential for chronic vasculitis management. This includes frequent check-ups, monitoring disease progression, adjusting treatment plans as needed, and addressing any new symptoms promptly. Consistent medical oversight helps optimize patient outcomes, prevent complications, and ensure ongoing disease control.
Potential Complications Arising from Untreated Vasculitis
Untreated vasculitis can lead to serious complications such as organ damage, blood clots, aneurysms, and stroke. Chronic inflammation from unmanaged vasculitis can result in long-term issues affecting vital organs like the kidneys, lungs, or central nervous system. Early diagnosis and appropriate treatment are vital in preventing these severe complications and preserving overall health.
Long-Term Effects on Organ Function
Chronic necrotizing vasculitis can lead to persistent inflammation that damages blood vessels and reduces blood flow to vital organs. Prolonged organ dysfunction may result in conditions like chronic kidney disease, pulmonary hypertension, or neurologic deficits. Proactive management and regular monitoring are essential to mitigate long-term organ-related complications and maintain optimal organ function.
Dietary Modifications and Exercise Recommendations
Vasculitis patients may benefit from a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to support overall health and immune function. Regular, low-impact exercise can help maintain cardiovascular fitness and reduce inflammation. Consultation with healthcare providers is crucial to develop personalized dietary and exercise plans tailored to individual needs and limitations.
Stress Management Techniques
Stress management is key for vasculitis patients to reduce inflammation triggers. Techniques like mindfulness, meditation, and deep breathing exercises can help alleviate stress. Additionally, engaging in relaxing activities, maintaining a healthy work-life balance, and seeking support from loved ones or counseling services can contribute to overall well-being and quality of life.
Current Developments in Therapeutic Approaches
Ongoing research is exploring novel treatments for vasculitis, including targeted therapies, personalized medicine approaches, and immunomodulatory agents. Advancements in understanding the underlying mechanisms of the disease aim to develop more effective and tailored treatment strategies. Clinical trials and collaborative efforts drive progress in improving outcomes and enhancing the quality of life for individuals with vasculitis.
Promising Areas of Research for Future Treatments
Future treatments for vasculitis focus on innovative approaches such as precision medicine, gene therapy, and immunotherapy. Investigational studies aim to target specific pathways involved in vasculitis pathogenesis, ultimately enhancing treatment outcomes and minimizing side effects. Collaborative research efforts continue to explore new horizons in vasculitis management, offering hope for more efficient and personalized therapeutic interventions in the future.
Patient Support Groups and Online Communities
Joining patient support groups and online communities can provide valuable emotional support, educational resources, and a sense of community for individuals living with chronic vasculitis. These platforms offer opportunities to share experiences, exchange coping strategies, and access updated information, fostering a supportive network of individuals facing similar challenges. Connecting with others can help reduce feelings of isolation and empower patients in their healthcare journey.
Professional Counseling and Mental Health Services
Professional counseling and mental health services play a crucial role in addressing the emotional impact of chronic vasculitis. Qualified therapists can provide tailored support, coping strategies, and mental health interventions to help individuals manage stress, anxiety, and depression related to their condition. Seeking professional help enhances overall well-being and resilience in navigating the challenges of living with vasculitis.